
How Bright Light Therapy Helps with Low Mood, Sleep Problems and Jet Lag
Last Revised November 2019

How Bright Light Therapy Helps with Low Mood, Sleep Problems and Jet Lag
By Daniel F. Kripke, M.D.
Last Revised November 2019
Happiness Needs Bright Light
Think about a person who has Seen the Light. Think about brilliance. Think how we describe the scintillating joy of love by singing, “You are my sunshine.” We know that light makes us happier.
Take a rose or a petunia indoors and it will wilt. Bring a peach or an apple tree indoors and you will get no fruit. Only a few houseplants will flourish indoors. People are similar. We wilt in the dark. Think about the dark dungeons of despair, the heart of darkness, the gloominess of a funereal mood. This language tells us what people have always known. Sadness rules where it is dark.
People were designed to be outside. It is part of what makes us human. Perhaps somewhere back in evolution, our ancestors may have resembled monkeys or chimpanzees that climbed trees and lived in dark forests. For example, the “Gorillas In The Mist” lived in a gloomy rainforest. In contrast, as our ancestors became human, they moved out more into equatorial fields and savannahs, became able to run further, and started looking about further for food. Some seasons had clear bright sun every day and some had rain, but it was always bright near the equator where they lived. Much of the time, there was hardly even partial shade. Our modern human ancestors became intelligent in places that were indeed very sunny. It is for such a life that our bodies are adapted.
When people settled down, about the time that recorded history began, our ancestors were still outdoors people. The men were outdoors hunting, fishing, farming, and fighting. The women were outdoors farming also, when they were not gathering food, grinding grains, weaving, cooking, or doing other things done mostly outside. Humans still spend much of their time outdoors where many people live: in China, in India, and in many of the tropical developing countries. Indoors, our moods start to wilt.
1.A. Modern people get less light
Only in recent generations, as society urbanized, did people begin spending most of their time indoors. Even in my lifetime, we have moved more indoors. As a little boy, I went outdoors every day to play, even in the winter. I walked to school and back, whereas more contemporary children ride. When television arrived, kids came indoors more, but we still played outside, because the attraction of the fuzzy black and white tube or the radio of my boyhood years was hardly comparable to entrancing modern television selections. How different it is today, when people of every age group spend so many hours watching television. With often hundreds of channels on the cable or satellite, there is always something fascinating for every taste. Big screen color has extra attraction, also. As if that weren’t enough, along came video games, and even more recently (for most of us), tablets, the Internet, and movie downloads. The result is that we spend more and more time in front of the tubes and less and less time in daylight. The tubes may seem bright, but the reason that we often watch them in dark rooms is that most give off very little light.
There is another problem in the cities of today. When I was a boy, I used to feel safe walking down Fifth Avenue in New York City. As a medical student, I walked at night in every part of the city. People no longer feel as safe. Older retired people, especially elderly women, may no longer feel safe walking around the big cities or going to the parks. The result is that older people are spending more time indoors. Construction of more indoor health and exercise facilities may be another factor keeping people indoors.
To gain more understanding of the lighting which contemporary Americans experience, my colleagues and I have measured how much time people spend outdoors in San Diego. We have studied a random population sample. It appears that in San Diego, California, people are outdoors in daylight less than one hour per day on average.[1] It is true that some people are outdoors for hours, working outdoors, shopping, playing golf, strolling on the beach, or whatever, but these people are not average. There are an impressive number of people who are in daylight only ten or twenty minutes a day or even less. Some San Diegans go through most days experiencing no daylight at all, besides which, sometimes they experience only dim indoor lighting.
We have found several factors which determine how much bright light people experience. The proportion of time spent indoors or outdoors is the most important influence. Season is next important, influencing the duration and brightness of daylight and the comfort of outdoor activities. As might be expected, people in San Diego experience almost twice as much light in the summer as in the winter.[2] Daylight savings time seems to be as important a factor as season itself, though season and the time standard are difficult to separate. We have found that volunteers from San Diego minority groups experienced somewhat less light than people of European ancestry, and women were outdoors less than men.[3] However, somewhat to our surprise, we have found that in San Diego, women from age 20 to age 80 years seem to experience rather similar amounts of daily light.[4]
San Diego is one of the most pleasant coastal cities in Southern California. We have more sunny days than 80% of American cities. Moreover, in San Diego, it is rarely too hot or too cold to be outdoors. Phoenix has more sunshine than San Diego, but if you ever walk around downtown Phoenix in the summer, you will find few people outdoors. In hot climates like Phoenix, people with air conditioning find it more comfortable indoors in the daytime. More widespread use of air conditioning may also be a new factor keeping more people indoors.
With colleagues, we compared people’s light exposure in San Diego with the pattern in Rochester, Minnesota.[5] Rochester is a charming small city in a rural farming area. In the summer, people in Rochester were out in daylight a bit more than in San Diego, perhaps because summer days are longer further north, or perhaps because more were busy with farming. In winter, on the other hand, people in Rochester were in daylight less than one third as much as in San Diego. The shorter winter days in Rochester are not the main reason that Minnesota people experienced little daylight. Most of the winter, Minnesota was just too cold for most people to stay outdoors more than they absolutely had to. In larger cities, people might see even less daylight than in Rochester, because Northern big cities are now built for traveling underground. In cities like Toronto, a person can take the subway to work and walk for blocks underground to arrive at the office or shopping without ever setting foot outside.
1.B. Lighting measurement
Our eyes adjust over such an astonishing range of lighting, that it is hard for us to realize how much brighter it is outdoors than indoors. Because your sensation is a poor judge of brightness, modern cameras contain light meters called photometers to measure brightness. The camera photometer tells you that your camera might need a one-second exposure for an indoor shot (without flash), when the same camera would capture an outdoor scene in 1/1000th of a second. That would be a thousand-fold difference.
Consider what scientific photometers tell us about the brightness of our varied environments. Modern photometers measure lighting in a measure called lux. Lux is a measure of how brightly things are illuminated. One lux is approximately as bright as the illumination from a candle one meter away in a dark room. An older measure, one foot candle, is the illumination produced by a standard candle one foot away. Since lighting diminishes as the square of distance, and one meter is a bit more than three times one foot, illumination one meter from a candle is less than 1/10th of the illumination at one foot. Thus, one lux is .0929 foot candle. Similarly, illumination at two yards (six feet) is only 1/36th as bright as at one foot, and lighting ten feet from a candle is only about 1/100th of the lighting at one foot (or 0.01 foot candle). The brightness 30 feet from a candle in a dark room is about the same as 0.001 lux, which is the brightness of starlight on a moonless night. When we distinguish shapes in starlight, we are seeing in only 1/1000th of one lux, which is about the darkest light in which we see anything.
In contrast, on a bright summer day when the sun is overhead, the brightness looking horizontally toward the horizon may reach 10–20,000 lux. It may get a bit brighter on a sandy beach or a snowy ski slope, but few eyes can stand more than 20,000 lux even briefly. Many people will put on sunglasses before it gets to 10,000 lux, so such people never expose their eyes to more than 3000–5000 lux. You may have heard that daylight reaches approximately 100,000 lux at noon on a clear summer’s day, looking straight up at the sun, but if we value our eyes, we never look directly at the noonday sun. Therefore, 10–20,000 lux is about the maximum that our eyes experience in sunlight. In summary, the human eye has the adaptability to see in a remarkable range of lighting. We can see throughout a visual range of more than seven orders of magnitude (2 X 107) or 20 million fold, from 0.001 lux to as much as 20,000 lux falling on our eyes.
1.C. Our lighting experience
Many scientists do not realize the dimness of indoor lighting, because illumination engineers often teach that indoor lighting is typically 100 to 500 lux. The engineers are thinking of bright offices and shopping centers (which are often especially brightly lighted), and they are measuring the lighting with their photometers pointed toward the ceiling lights where we rarely look. If we measure in the directions in which eyes usually look, we have found that most indoor settings are much dimmer than 100 lux. A fashionable living room might be 20 to 50 lux or less. A fashionable bar or restaurant could be as dim as 1–2 lux. In a lecture hall where scientists watch slides, 1–2 lux is about average. Movie theaters are darker than one lux. Thus, it could be 1,000 or even 10,000 times brighter outdoors in daylight than indoors.
A big surprise for us was to discover in what very dim light people often watch TV. In a recent study, the mid-range subject averaged 31 lux in the evening, but some people’s TV rooms are only about 1 lux (about the same as the light of a full moon).[6] That is dark! Please do not think that the TV screen itself is very bright. Most TVs may appear bright, but they do not light up a room. Usually, you could not read comfortably by your TV’s light alone.
Because of the huge range of different lighting conditions in which we can function, an extremely wide range of lighting experiences is possible. We used a special instrument called an Actillume to measure how much illumination people actually experienced. Worn on a wrist, Actillumes measured both activity and illumination (Acti… + illum…) It was invented in our San Diego laboratory with the assistance of the late Mr. William Gruen of Ambulatory Monitoring, the company which manufactured and sold this instrument. The Actillumes could measure lighting (exactly like a camera light meter or photometer) and store the results every minute for several weeks in its internal computer memory. In measuring a randomly-selected group of 318 San Diego volunteers from 40 to 64 years of age, we found that in the course of a two-day recording, the volunteers who received the brightest illumination (spending bright days outdoors) were experiencing as much as 1,000 times the 24-hour light exposure of those who received the dimmest lighting.[7] Evidently, those receiving the dimmest lighting never went out in daylight, and even indoors, their rooms were lit more for TV than for reading. We were quite astonished to learn that different people experience a thousand-fold range of lighting. Such differences must have many effects.
More recently, quite a few wrist mounted and body-mounted instruments have been developed to record the illumination that a person is experiencing. You can monitor your light exposure with some special smart watches as you can now monitor your pulse rate. There are some problems because a wrist-mounted light sensor is often not aimed in the same direction as the eyes. Also, at night, either the light sensor or the eyes may be covered by pillows or bedclothes.
The averaged light exposure over 24 hours for the median San Diego man was 350 lux, with only 278 lux for women. Since much of the night was spent near zero lux, time awake may have averaged close to 500 lux. That does not mean that most of the day was spent in 500 lux – to the contrary, to achieve an average of 278–350 lux, a short time (e.g., usually under one hour) was spent in bright daylight of several thousand lux, and much of the rest of waking time (even during the daylight hours) was spent in less than 100 lux.
Below the median daytime illumination, we have found that more people report depression. For some people, less than an hour of daylight seems insufficient to uphold their mood and may be a cause of depression.
Depression and the Droopy Dims
Depression is increasing, according to some studies.[8] Sales of antidepressant drugs have been steadily increasing.[9] As far as psychiatrists can tell, there is more depression today than there was a generation or two ago.[10] Depression seems to be starting at an earlier age. The suicide rate is higher among teenagers and young people. Perhaps illegal drugs, opiods and sleeping pills, are factors in increasing suicide today, but it could also be that depression is causing more drug and alcohol use. The rate of suicide has also been increasing among the elderly.[11] Depression is more of a problem in urban areas: the depression rate is lower in rural areas, where people may go outside more to work.[12] In summary, depression and suicide are increasing, possibly in part because people are experiencing less daylight.
What is depression? Part of depression is a gloomy feeling at times of loss – when we lose a job, a friend or have other disappointments. Some of the most serious sadness comes when we lose a loved one such as a parent, spouse or child. Such sadness is normal (in the sense that we all experience bereavement, not in the sense that losses are not painful). Such sadness is often psychological in origin, and since bad experiences fade away, such sadness usually gets better by itself. But recovery may be agonizingly slow. Further, there are other kinds of depression more biological in origin.
Some people – before the end of their lives about 15% of Americans – experience at least once what we call a major depressive disorder.[13] A major depression is so much depression that the person feels depressed, down, sad, or gloomy most of the day nearly every day, or loses interest in normal pleasures. Moreover, by definition (for a depression to be “major”), the person with major depression has at least three or four additional symptoms such as loss of weight or gaining weight, loss of sleep (or sleeping too much), becoming agitated or slowed down, becoming fatigued, feeling guilty and worthless, losing the ability to concentrate, and actually thinking about death or suicide. We call it a minor depression if there are fewer symptoms. We call it a dysthymic disorder if the symptoms are milder than major depression but persistent with little let-up for at least two years or more. Some might not consider mourning and bereavement as a “complicated bereavement disorder” unless the disturbance remains severe for at least six months, or unless it becomes so severe that the bereaved person is in danger or suicidal.
If major depressions happen at least once in a lifetime to 15% of us, the milder depressions such as dysthymia, minor depressive disorders, and other grumpy moods may occur in an additional group of almost equal size.[14] Among older people, especially above age 70 years, the kind of depression characterized by feeling worn out, depleted, and tired is particularly common, even though this is not called a major depressive disorder.[15] Nevertheless, minor depression in the elderly can be quite disabling. Almost all depression among elderly people is accompanied by sleep disturbances. As a matter of fact, sleep disturbance is often a warning sign of impending depression.
There is another kind of usually-mild depression found especially among women before the menopause, which tends to occur in winter. We call this “seasonal affective disorder” or SAD, which in most cases is another name for winter depression.[16] Oddly enough, people with seasonal affective disorder often say that they sleep more than usual, although it may be more a matter of feeling fatigued and spending extra time in bed rather than actually being asleep. Another peculiarity of SAD is that people with this problem often have particular problems in getting up in the morning. In more severe cases, they may have a clearly delayed sleep phase, that is, they both have trouble falling asleep until late (e.g., long after midnight) and they also wake up late. Some delay in sleep patterns is usually found in the average patient with major depression,[17] but is particularly prominent in SAD. Among older patients with nonseasonal depressions, waking up early is common, but early awakening can be found in SAD also. Many people with seasonal affective disorder experience increased carbohydrate craving such as eating sweets, and they sometimes gain weight and need larger clothing in the winter, though loss of appetite is also common in SAD. Some people with SAD feel withdrawn and want to curl up like a hibernating bear, but they may have fewer symptoms of sadness and guilt than other major depressives. Like other forms of depression, there is a milder form of SAD called “subsyndromal SAD” which is simply less severe, but it is more common. People with the milder seasonal disorder suffer mild lethargy, gloom, or weight gain in the winter, sometimes oversleeping in the mornings, but not a really disabling depression.
It seems quite clear that many people with SAD have the winter pattern of recurrence at one time in their lives and the more common nonseasonal pattern on other occasions.[18] In my opinion, both seasonal and non-seasonal depressions are probably somewhat different manifestations of the same illness, just as some people with measles have more spots on the face and others have more on the body. Some people have just one depression in a lifetime, but probably for most people with depression, depression is at least occasionally recurrent. The pattern of those recurrences is extremely unpredictable for most people with depression. Most major depressions do not occur in the winter. In fact, there may be more depression in the spring (and perhaps in the fall) than either in winter or in summer.
We now know that depressions occur more often among people who do not get enough daylight – who do not experience enough bright light. Among the randomly selected people in San Diego who volunteered to wear an Actillume, the trend was for people who experienced less bright lighting (largely because they spent less time in daylight) to report more depression.[19] In San Diego, there is only a small difference in available daylight between summer and winter, so the relationship of low light to depression could not be explained by the winter season. On the other hand, winter depression becomes increasingly common as one examines the more northern areas of the United States, especially Fairbanks and northern Alaska. It is very clear that as one moves north – and arrives at places with shorter, darker winter days – the prevalence of winter depression increases. Cold winter temperatures are also related to winter depression, which may suggest that part of winter depression is caused by cold weather keeping people indoors. As might be expected, the pattern of recurrent summer depression seems to be most common in the hottest parts of the U.S., though it does not seem as common as winter depression. It may be that summer temperatures which keep people indoors in air conditioning (and out of daylight) are an explanation for summer depression.
Treating Depression With Light
Here is good news for depressed people! You can often make yourself happier simply by lighting up your life! With some advice from your doctor, you can relieve depressive symptoms by getting more bright light. Just as darkness makes us sad, bright light tends to restore us to a normal level of cheer. This simple and very helpful principle helps us escape depression.
You can help depression by spending more time outdoors in daylight, but to be frank, changing habits to experience more daylight is often not practical in today’s urban societies. That is why we usually recommend increased artificial lighting. This section will explain how you can use bright light treatment, but if you have significant depression, you should also check with your doctor.
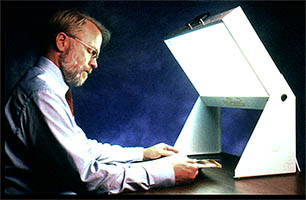
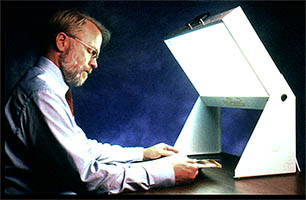
3.A. Dosage of light
People vary in how much bright light they need to combat depressive symptoms. There must be many factors, especially how depressed a person is. A modest increase in lighting may help with a mild problem. A more severe problem may need much brighter lighting and a longer duration of bright lighting to overcome. The amounts of light needed should at least bring a depressed person above the average for daily light exposure. This can be achieved with as little as 30 minutes of very bright light near 10,000 lux (like sunshine) or with a couple hours of light of about 2500 lux (like a cloudy day or deep shade).
If the amount of depression is substantial, light much dimmer than 2,000 lux may not be very effective without many hours of daily exposure, though in the chapter on advanced sleep phase, I will describe how modest amounts of lighting may be sufficient for certain sleep problems. We have to admit that the information doctors now have about the effectiveness of different lighting dosages is quite fragmentary. We really cannot give very exact advice about what brightness and duration of light a particular person should use. (Incidentally, doctors have a similar problem in recommending the dosage needed of antidepressant drugs or the amount of psychotherapy needed.) Thus, for the present time, somebody who wants to use bright light might need to try to experiment with how much light is needed.
Using light treatment for up to several hours a day might be beneficial at the beginning of treating serious depressions. Most people would be able to decrease the duration of treatment after a satisfactory response was obtained. Initial durations of 30 min. for 10,000 lux or 2 hours for 2–3,000 lux are often satisfactory.[20] There is some evidence that much less light may be needed when the blue and blue-green wavelengths are augmented,[21] and brief exposures to flashes of bright light may work as well or better than long exposures.[22] See the discussion of choices of lighting below, but much more research about these factors is needed before I could recommend more limited exposures to bright white light.
I would be uncertain of the safety of increasing the brightness of light treatment above 10,000 lux, so I never recommend any brighter treatment.
The decision about whether to try 10,000 lux for a shorter time or 2,000–3,000 lux for a somewhat longer time depends on several considerations. Most people prefer the brighter light for the shorter time because of the convenience of shortening the time required. However, using 10,000 lux does generally require getting close to the light source, which may be awkward in some settings where it is convenient to use a lower intensity for a longer time. A full 10,000 lux will also make some people’s eyes uncomfortable or increase headache and eyestrain. Theoretically, we would expect 2,000 lux to be safer for the eyes than 10,000 lux, but 10,000 lux has been tested enough now without causing any consistent eye damage that most experts seem quite confident of its safety. After all, 10,000 is no brighter than what we normally experience when we spend time outdoors on a bright day. People have been testing 10,000 lux for longer than recorded history. I will describe just how to provide this bright light in another section below.
Like many other habits – eating, exercising, and sleeping, for example – a person may need to try different amounts of bright light to discover how much is best individually. If a half hour a day is not doing enough after a couple of weeks, try one hour or two hours. If 2000 lux is not doing enough, try 10,000 lux. Although some people will experience some mood improvement within an hour of a single dose of bright light, it often takes a week of daily bright light treatment for a severely depressed person to feel a measurable improvement, and increasing benefit may be felt as treatment continues for at least eight weeks. Unfortunately, we do not have adequate controlled trials of treatment longer than eight weeks, but that is true of many antidepressant drugs as well. It is likely that continuing improvement or prevention of relapse will continue for many months. One should not become disappointed too quickly, especially if even slow improvement is seen. On the other hand, it is possible to use too much bright light. The dosage in time or brightness sometimes needs to be adjusted and reduced. Eyestrain, headache, irritability, and sleep problems may be signs of excessive treatment. In a later section, we will consider some specific side effects on sleep and mood which may require reduction of dosages.
3.B. The time of day to use bright light
For many people, bright light at any time of day will help depression. It appears that most people will get the best benefit from bright light very early in the morning, even starting an hour before the person's usual time of awakening. However, there is a smaller group who seem to benefit more with evening light. I think it is the sleep pattern which provides the most practical clinical clue to optimal timing.
The principles for optimizing light timing from sleep patterns are simple. If a person tends to have trouble falling asleep and has trouble getting up on time each morning, that person is likely to do best with using bright light soon after awakening. People whose depression is linked to sleeping more may also tend to do best with light in the morning. For such people, using bright light immediately after awakening is the most effective time to use bright light. Indeed, some studies suggest that getting up an hour or two before usual awakening to use morning bright light increases its benefit. Dr. Terman recommends beginning morning light treatment about 2 ½ hours after the middle of sleep.[23] For example, if a person sleeps from midnight to 8 am (with midsleep at 4 am), the recommended treatment-start time would be 6:30 am. In contrast, evening bright light may be best for the person who tends to nod off early in the evening, who cannot stay awake for prime-time television, and who awakens earlier than desired in the morning. For the person who does not fit clearly into either of these patterns, there might be little difference between morning and evening bright light treatment, but morning light would be the better bet. We will explore these principles in more detail in the section on advanced and delayed sleep phase syndromes.
For the person suited for morning light, a way to get fast relief is to use wake therapy. The way to use wake therapy is to get up in the middle of sleep, turn on bright room lights, and stay entirely awake for the second half of the night (e.g., a person who sleeps from midnight to 8 am would get up about 4 am). Then, bright light treatment is commenced near the normal awakening time. Most depressed people experience surprising first-day relief of depression after getting up so early, provided they stay awake all day despite some increased sleepiness. Although patients who are not using bright light tend to relapse after wake therapy as soon as they sleep again, if bright light treatment is immediately added, the rapid gains of wake therapy are often maintained. I believe that a single night of wake therapy (getting up in the middle of the night) is helpful and practical at the beginning of light treatment. Getting up a bit early thereafter might also help.
A few researchers have reported faster and more powerful benefits from a triple therapy involving part-night or full-night wake therapy, moving subsequent sleep intervals earlier in the night, and bright light.[24] Though the results are impressive, in 2019 I still do not know of a well-controlled randomized trial proving that triple therapy works better than bright light alone.
A special case are the patients with bipolar disorder (a history of being manic depressive), especially those whose moods cycle rapidly between mania and depression. These patients may possibly be prone to trigger unwanted and serious mania with use of bright light, especially in the morning, or with wake therapy. Mid-afternoon bright light may be the best for these patients, according to preliminary testing. [25] Because of the risk of mania, I do not recommend wake therapy for bipolar patients, unless the patient is actively supervised by a doctor.
Please see below, in Chapter 7, the warning against manic-depressives using light or wake therapy without a mood stabilizer.
3.C. Choices of lighting
The most important aspect of treatment lighting is that it be bright. So far as we know, sunlight and artificial lighting might work equally well if the artificial light contains the right wavelengths (colors). However, in various climates, environments, and social situations, using sunlight may be impractical, so most people will need to buy, rent, or borrow special artificial lighting. So far as we know, both ceiling lighting that hits the eyes and lighting level with the eyes work equally at the same brightness. There is some indication – not yet proven clinically – that light coming from below the direction that the eyes are looking (e.g., a light on the floor) would not work as well.
So far as we know, diffuse incandescent and fluorescent light of equal brightness might work equally, but there are two important advantages with fluorescent fixtures. First, since fluorescent lighting is more energy-efficient, you pay for less electricity and produce less wasted heat with fluorescents. That heat could be annoying in the summer. Second, fluorescent tubes are large, so it is easy to diffuse the light over an area of several square feet. This means that unlike the very bright point of light produced by incandescent bulbs, fluorescents produce somewhat dimmer light over a larger area. When the light goes through the lens of the eye and hits the retina (the back of the eye), the energy of diffuse light is spread over a large area, so it should not heat the retina or make you see spots (like the spots you see after looking at a flash bulb). Diffused bright light is safer for the eyes and will cause less strain. As a general rule, you could not burn your retina by staring at any of the common fluorescent bulbs with diffusers, even if you are receiving 10,000 lux. Obviously, nobody should stare at a light if it hurts or seems to dim the vision. Some people are annoyed by the flicker or sound of older fluorescent ballasts, so fluorescent fixtures with electronic (high frequency) ballasts will probably cause less headache and sense of eye strain. Avoid the older models flickering with the 60 cycles household alternating current.
I am not certain that staring at very bright incandescent bulbs is entirely within the range of safety. I would never recommend that anyone take any unnecessary chances with their eyes, so I feel that nobody should treat themselves by looking directly at bright incandescent light (such as 300-watt halogen bulbs) without diffusers. Indirect incandescent lighting or lights with large diffusers or shades should be safe, as I will discuss in the section about using lighting for the elderly. The problem with using indirect incandescent lighting for treating depression is that the standard commercial lamps lose most of the brightness by bouncing the light off the walls and ceiling, partly because the light travels a greater distance. As a result, the lighting store “torchiere” incandescent lamps are probably not bright enough to do the job well for serious depressions. Another problem is that the 300–500-watt halogen incandescent bulbs used commonly do not last very long and may be a bit difficult to replace. For many years, all of the lighting fixtures which I recommended for significant depression used fluorescent bulbs and diffusers.
Recently, there have been technologic developments in LED lighting. LEDs are even more energy-efficient than fluorescent bulbs, and they will last longer. However, except for a few studies with the “Litebook” brand LED devices, which have been shown to have beneficial effects as compared to placebo, there has been relatively little testing of the white LED devices. Some of the products such as Litebook models use LEDs to produce intense white light from a rather small area, which might produce more glare or discomfort. LED lighting may potentially provide a more therapeutic, safer, and more practical kind of light treatment than fluorescent alternatives, but I have not yet seen evidence that is clinically persuasive. I am not aware of sufficient testing to make me as confident of these LED treatment devices as the fluorescent designs unless the LED light is diffused over an area of a square foot or more. The truth is, there have been virtually no controlled comparisons available between different models and brands. Even brands shown to be effective change the design of their products so rapidly that it is hard to be sure which current models are adequate.
New research has shown that the “photometer” cells in the retina of the eye that respond to brightness (the intrinsically photosensitive retinal ganglion cells) are most sensitive to blue and blue-green light. These cells contain a special visual pigment called melanopsin which responds best to blue. On the other hand, there also seems to be a benefit in additional colors of light, such as some green mixed with the blue, perhaps reflecting input from rod and cone photoreceptor cells to the intrinsically photosensitive retinal ganglion cells. The issue is complicated by the fact that the lenses in our eyes turn yellow as we age, so that blue light does not reach the retina of older adults as well as green, yellow or red. There have been several studies which suggest that blue LED light of only moderate intensity will influence the circadian system more than white light of the same intensity. However, in 2019, it remains unclear how much this advantage of blue light is observed among older adults and if blue light has any advantage in treating depression. The hope is that blue LED light which seems less bright and requires less electricity could be as useful as brighter white light, but I have not seen adequate clinical proof. Although the blue LED devices are thought to be safe, their margin of safety may not be as great as with white light, because animal studies show that blue light can be much more damaging to the retina. All in all, as of 2019, I am inclined to feel more confidence with the white fluorescent and white LED models.
There are now a large and confusing number of light treatment models and manufacturers advertised on the internet. Several manufacturers (listed in the box below) make fluorescent fixtures which have done a very nice job of helping depressed patients. A good place to find lighting manufacturers is at the website for the Society for Light Treatment and Biological Rhythms.[26] In general, 160–300 watts of fluorescent light illuminating a bright diffuser about 1 yard from the eyes will give about 2,000–3,000 lux. The exact brightness depends on various aspects such as the bulbs, the diffusers, and the reflectors. To get 10,000 lux, the manufacturers may recommend a somewhat bigger fixture with more wattage or placing the fixture closer to the eyes, perhaps 12" to 18". There is considerable difference in the brightness of different models, so the dimmer models may need to be closer to the eyes. Some of the designs hold the light tilted a bit above the eyes, which seems to be convenient for getting light treatment and at the same time getting something done reading, writing, eating or watching TV.
Some researchers have recommended that people stare at the fluorescent diffuser most of the time when they are getting the treatment. Others have recommended glancing at the light every minute or two. Others seem to feel that having the light source anywhere in the field of vision (even if you aren’t looking at it directly) is just as good. Unfortunately, we really do not know yet whether it makes much difference how much you look directly at the lighting. Most evidence suggests that having the light within the field of vision and glancing at it occasionally will be sufficient. Also, unfortunately, we really do not know what difference it makes where the light is during treatment: above the eyes (tilted), straight in front, to the side, or even below where the person is looking. There is some evidence – not fully convincing – that light slightly above or even with the eyes would be more effective than light coming from below where the eyes are looking.
I wish we had some sort of independent testing of different brands and models of bright lights, to see which ones helped depressed people the most. We do not. Comparative testing would be difficult and expensive, so almost none has been done. There is much depression and suicide among families with incomes of tens of millions of dollars or more every year. One would think some of these very wealthy families would want to contribute to getting the needed testing done. Please do not suppose that the need for more information is limited to light treatment of depression. We likewise need more information comparing different types of antidepressant drugs used in various circumstances, different doses, and different timings and durations of drug administration. It would be laughable to imagine that we have much information comparing different psychotherapists or the ideal dosage (number and timing of visits) for each psychotherapist. In some ways, our knowledge about light treatment of depression exceeds that for alternative treatments.
A lot has been written about natural lighting and whether one should use lighting with a “full” spectrum. I suspect this spectrum of claims is largely baloney! In fact, the FDA forced one company advertising “full spectrum” light into a consent decree admitting that their claims were deceptive.[27] First of all, almost any white light produces the full visible spectrum of colors (light wave lengths). The question is the balance of the different wavelengths, which does differ from one light source to another. If one looks at the fine spectrum with a precision spectrophotometer (which measures the color balance of light exactly), I doubt that any of the commercial sources really produces a light spectrum which could be mistaken for the rather smooth spectrum of natural sunlight. Fortunately, the eye is not a spectrophotometer, and there is no evidence that the sunlight spectrum is necessary.
The main issue is how much ultraviolet light the light source produces, because some of the “full spectrum” bulbs give off enough ultraviolet to possibly increase cataracts, retinal damage, or skin cancer. There is no evidence that the ultraviolet is needed for the bright light treatment benefit, so needless to say, I do not recommend anything with significant ultraviolet. Most of the fluorescent manufacturers use a plastic diffuser which filters out the harmful ultraviolet. There is more discussion of the risks of ultraviolet in the chapter about risks. It is true that many Americans get so little ultraviolet sunlight in the winter that they become vitamin D deficient, especially when fear of obesity unwisely persuades people to avoid Vitamin-D-fortified dairy products. It is sun striking the skin, not the eyes, which helps with Vitamin D, so if you are going to a tanning salon for Vitamin D, keep the ultraviolet out of your eyes. Then light up your eyes without the ultraviolet. Anyone concerned about vitamin D would probably be wiser to buy some in the grocery store than to try ultraviolet lighting to prevent vitamin deficiency. Dairy products can be good for you. Did you know that you might actually get depressed, if your cholesterol is too low?
There has been a good deal of hoopla and advertising about light visors. The idea is that if you could wear the light source on your head like a baseball cap – and get bright light treatment without blinding yourself – it might be easier to go about your business. I have never recommended light visors, because for many years there was no evidence that such visors worked for treating depression. In fact, there had been several studies suggesting that various light visors which have been tested did not work better than ineffective dummy treatments. Recently there have been some promising reports about new kinds of visors, but I do not know whether they can be recommended.
Apparently a more promising approach to making light treatment easy is providing light exposure during sleep. There is some evidence that gradually increasing light toward the end of the night, simulating dawn, has a useful effect.[28] I do not think that the dawn simulation idea has yet been proven superior to applying a steady intensity of light during sleep. There has not yet been sufficient research on this technique from different laboratories. I do not favor dawn simulation unless it is quite impossible to arrange for sufficient light when you are awake, but some manufacturers provide dawn simulation devices, if you want to take a chance on trying light before waking up. Light before waking up is a form of morning light, and it probably will work best for people with trouble falling asleep and with trouble getting up on time.
Light Box Suppliers I Recommend:
Center for Environmental Therapeutics, www.cet.org![]()
![]()
Enviro-Med, www.bio-light.com![]()
![]() , (800) 222-3296
, (800) 222-3296
The Sunbox Co., www.sunbox.com![]()
![]()
Nature Bright, www.naturebright.com![]()
![]()
For more information about light, try the Society for Light Treatment and Biological Rhythms (SLTBR), www.sltbr.org![]()
![]()
3.D. Using light for the long run
If you tried bright light and you felt better, what do you do next? Many people should keep using light. Often, our need for bright light is not temporary. Depression may be a long-lasting problem, not temporary like a sore throat. If you need supplemental light, you may need light supplements for years, or at least until your habits change. You would not expect your need for food or exercise or sleep to be temporary. You would not expect a rose bush to need time outdoors only occasionally. For rose bushes, light can be a life-long need. For some people, a need for light might also be life-long.
Therefore, some people who benefit from bright light need to use bright light almost every day for years. If they stop using light, after a few days or weeks, they may relapse and become depressed again. We do not think the need for bright light is like the addictions, where addicts must increase their doses as they develop tolerance. In fact, people often find that they need less time with their light box to avoid relapse than they did initially to make the depression go away. Perhaps light is like taking aspirin for arthritis: if an arthritic stops taking the aspirin, the old joints could start aching again! Perhaps for some people, using light may be like taking insulin for diabetes: if a diabetic stops taking the insulin, the blood sugar problem is likely to reappear.
If a person has been depressed for the first time, and after using bright light has felt well for a good time (not less than two or three months, I would think), it could be reasonable to try slowly reducing the light dosage, to see if symptoms recur. You should think twice about reducing the dosage if your mood is not completely satisfactory, and you are still having some depressive symptoms, because then relapse is more likely. Be alert to the possibility that you could reduce your lighting dosage and feel well at first, but that relapse of depression could occur weeks or months later. Restoring light dosage might become necessary even several months or more after light treatment is cut down. It would be safer for most people to cut their light dosage in half for at least one month before stopping bright light usage completely. An exception might be people with winter depression who have learned that their symptoms stop at a certain time of year. However, experience teaches that even winter depressives often need light year-round.
Using Antidepressant Drugs and Counseling
Remember the caution with which we started discussing light treatment of depression. You should check with your doctor. If you have significant depression, especially if you might have a major depressive disorder, if bad mood is keeping you from your normal activities, or you have any thought of hurting yourself, you should certainly get your doctor’s help. It is nice that self-managed light is sometimes sufficient for the mild problems, but please do not count on bright light alone if your depression is causing serious trouble.
This caution is similar to the caution with other health aids. An average person knows how to get some exercise, but if you have had a heart attack, you would need to discuss exercise with your doctor. An average person knows it is good to skip dessert, but if you have diabetes or a stomach ulcer, you need to discuss a detailed diet with your doctor. Similarly, people might try light for minor problems by themselves, but for serious depression, a doctor’s advice should always be sought.
We used to think about bright light as an alternative to the better-known treatments for depression, especially as an alternative to antidepressant medicines and counseling. That is not my viewpoint anymore. Experience shows that even when light treatment helps, it is often not enough. We realize now that light treatment works very well in combination with the antidepressant drugs. These are drugs like citalopram, amitriptyline, trazadone, and lithium – there are quite a few kinds which are good. In fact, it seems that bright light often works best along with antidepressant drugs. The benefits may multiply each other.
Requiring years of effort, a very carefully-designed randomizing controlled trial was done at psychiatric centers in Canada, comparing light treatment with placebo, with fluoxetine (one of the most popular antidepressants, e.g., Prozac brand), and with the combination of light treatment and fluoxetine.[29] The patients suffered nonseasonal major depressions. The outcome is summarized in the figure below: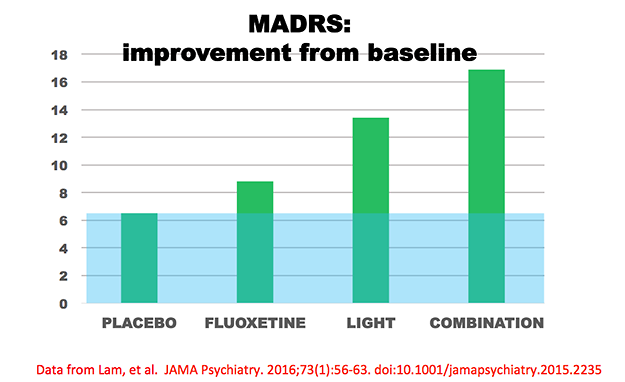
The MADRS is a quantitative estimate of the intensity of a patient’s depression. The figure above shows the amount that patients’ MADRS scores improved (depression scores decreased) from baseline to the end of eight weeks of treatment. The group that received only inactive placeboes improved 6.5 points, a typical combination of “placebo effect” and spontaneous remission in such trials. The blue shading shows this “placebo effect,” and the green bars extending above the blue show the amount the treated groups improved more than those with inactive treatment. The fluoxetine drug group improved 2.3 points more than the placebo group, a typical benefit size in controlled trials of fluoxetine. The light-treated group improved 6.9 points more than placebo, and the group receiving the combination of fluoxetine and light improved 10.4 points more. Note that the combined group experienced somewhat more benefit than the sum of improvements in the fluoxetine-alone and light-alone groups. To summarize this important study, not only was light treatment better than the no-treatment control, light also worked faster than fluoxetine and appeared to help more. Moreover, the combination of light treatment and fluoxetine was better than fluoxetine alone. Although the statistical analysis was not adequate to prove interaction, the combination of light treatment and fluoxetine appeared somewhat better than simple addition of the light-alone benefit plus the fluoxetine-alone benefit; that is, the two treatments appeared possibly synergistic and seemed to help each other. This study as well as other studies of combined treatment argue strongly for combining light treatment with antidepressant drugs.
There are some controlled trials assessing psychotherapeutic treatments versus light treatments versus their combination for SAD, showing possibly somewhat faster responses with light,[30] possibly more lasting freedom from relapse with CBT psychotherapy of depression,[31] but the best results with the combination. I think it appears likely that a combination of light and antidepressant drugs and CBT psychotherapy would be optimal.
I was formerly quite enthusiastic about the antidepressant medicines for outpatients. These medicines help millions of people. However, usage has grown so great that it is no longer clear that antidepressants are needed by everybody who is getting them. Moreover, recent critiques which examined the controlled drug trials that were not published (as well as the more favorable trials which the manufacturers published) have indicated that our appreciation of the antidepressant drugs may have become over-enthusiastic.[32] Realistically, for patients not depressed enough to be hospitalized, the amount of the benefit of the antidepressant drugs is usually very small. Nevertheless, depressed people in most cases do better with antidepressant medicines than without them. There have been literally hundreds of studies which prove that the antidepressant medicines provide more benefit than they do harm.[33]
Do not be scared by all the sensationalism about side effects which has appeared in certain news media. It is true that all antidepressant drugs have side effects, but so do water, sugar, salt, apples, oranges, and just about anything else in life. Compared to driving an automobile, much less a riding a bicycle or trying roller blades, antidepressant drugs are very safe. For most people who are really depressed, the side effects of antidepressant drugs are worth it. Talk to your doctor about it.
Counseling is also good for depression. There are new kinds of psychotherapy of depression that really do work. There have now been many studies which prove the benefits of modern psychotherapies of depression. A long time ago, I was trained in the old Freudian methods of treating depression (dream analysis and talk about childhood, for example), and I have to say that I do not believe that those old methods helped depression much. Doctors trained in the newer methods accomplish more. Psychotherapy certainly seems generally safe. In all probability, psychotherapy plus antidepressant drugs works better than the medicines used alone. There have been few good tests of the combinations of bright light and psychotherapy and no tests of combining bright light, medication and psychotherapy that I know of. There is every reason to think that these combinations would be safe and more effective than a single treatment. Indeed, the combination of bright light, antidepressant drugs, and psychotherapy might be the best for many people. I wish there were more results of clinical trials of light benefits to describe, but no treatment in medicine has been tested long-term in every possible combination with other treatments. Talk to your doctor about psychotherapy.
Bright light treatment for winter depression has been supported by dozens of studies demonstrating beneficial results (though there have been a few studies with unsuccessful results).[34] The Clinical Practice Guidelines issued by the U.S. Department of Health and Human Services[35] recognized bright light as a generally accepted treatment for winter depression.
Until recently, there were rather few studies of bright light treatment of nonseasonal depression; however, there are now dozens of controlled studies showing that bright light reduces symptoms in nonseasonal depression. The study of Lam et al. described above was the most conclusive study, but we might review some of the earlier ones.
Scientists rate how depressed patients are both before and after treatment using descriptive methods called depression rating scales. For example, a doctor who talked to the patient gives scores for how much the patient seemed sad, guilty, without appetite, suicidal, and so forth to add up a total depression score. One of the most widely used scoring methods is the Hamilton Depression Rating Scale or HDRS. Because depressed people usually recover spontaneously, given enough time, the depression ratings of patients who are given no active treatment usually drop over time. Thus, even when depressed people who volunteer for research studies are given an inactive placebo pill or placebo (inactive) light, their depression ratings decrease after eight to 16 weeks. In a clinical trial, volunteers are randomly given either the active treatment (such as bright light or an antidepressant drug) or the inactive placebo for contrast. To calculate how much of the average patient’s recovery was due to the active treatment, I considered the baseline depression rating (e.g., the HDRS score) as the 100% reference, and then the depression ratings at the end of the trial were computed for active treatment and for control treatment as a percentage of this baseline. Then, the net benefit of the active treatment was computed as the percentage reduction of depression ratings with active treatment minus the percentage reduction of depression with the control treatment.[36] Above, the figure of results of the Lam et al. study similarly display net benefit as a percentage reduction of MADRS score.
Our first studies of bright light tested only one single hour of bright light to treat hospitalized patients with nonseasonal depressions.[37] The patients were awakened to receive the light treatment from two hours to one hour before the patient’s usual planned time of awakening, so that these patients experienced one or two hours of wake therapy at the end of the night. We now call getting patients up early “wake therapy,” because to call this helpful treatment “sleep deprivation” gives the wrong impression. Most patients were drug free, but some were taking antidepressants during light treatment. As compared to a control hour of light placebo, which presumably produced the same sleep curtailment, the bright light reduced mood ratings about 12%. As will be explained, a 12% net gain as compared to placebo is similar to benefits achieved by antidepressant medications after weeks of treatment, so it was remarkable that such substantial benefit could be obtained with one single hour of bright light.
In an extension of our initial studies, 25 drug-free patients were treated with bright light each day for one week, compared to 26 patients treated with a dim-light placebo.[38] Depression ratings were 18% lower after bright light than after placebo, a benefit which was statistically significant. These and other data suggested that one-week treatment produced more benefit than only one hour of bright light. More recently, another one-week study of unmedicated inpatients observed a somewhat larger net advantage of 24.2%, which was likewise statistically significant.[39] Even a study reporting no statistically significant benefit achieved a 12.2% net advantage in HDRS ratings of the bright-light treated group[40], so that the failure to achieve statistical significance could have been partly due to an insufficient numbers of subjects. These studies of drug-free depressives were consistent in demonstrating advantages of bright light treatment.
Two European studies were important because they examined effects of bright light (as compared to a dim-light placebo) in patients who were also receiving antidepressant medications. In both of these studies, the net relative advantage of bright light over dim light was 27%. [41] Since the medication-only groups also did well in these combination studies, the additional improvement gained by the light-treated patients was especially impressive. A third European study also demonstrated substantial benefits of bright light compared with placebo among patients simultaneously receiving antidepressants.[42] Not only do these studies show that bright light improves the antidepressant response of patients who are receiving antidepressant medications, but they leave the impression that the benefit of bright light may be greater when patients are also receiving antidepressants.
A light triple treatment for nonseasonal depression was then tested.[43] Ironically, this new light treatment was developed by Dr. Neumeister working under Dr. Kasper at the University of Vienna – the same place where Sigmund Freud trained so many years ago. The Vienna psychiatrists treated patients in the hospital with serious nonseasonal depressions who were being treated with antidepressant drugs but had not yet responded. At the start, the doctors in Vienna awakened these patients in the middle of the first night and kept them awake for the rest of that night, while starting bright light treatment and also continuing with antidepressant drug treatment. About 70% of these patients felt dramatically better on the day after they had been awakened early, and they continued to feel better for the following days. About 35% of their depressive symptoms were relieved immediately. It had been previously known in Europe that such awakenings often relieved depression on the day of the early wakening, but the patients usually had relapsed almost completely the next day. Because of this relapse, few doctors in America thought that wake therapy was really very useful. If adding bright light can prevent the relapse, we have a new way to relieve the symptoms of severe depression in one day. There is nothing like it. This excellent response to bright light combined with wake therapy and antidepressants has now been reproduced by other studies at European hospitals.[44] Our group has also reproduced this effect in a small study of outpatients, who awakened themselves at 2 am in their own homes.[45]
Several studies have shown that bright light may be useful for depressed elderly in nursing homes.[46]
In addition to these studies, there has been one controlled study showing that 10,000 lux produced more benefit than 2,500 lux, when treatment was only 30 min. per day.[47] This study in effect confirms that bright light is an active treatment. Also, two studies have found shorter hospitalization times needed when depressed patients were in bright rooms than in rooms with darker windows.[48] A well-designed study showed that bright light was useful for premenstrual depression.[49]
There have been only three early studies with good scientific methodology which failed to confirm significant benefits of light for nonseasonal depression. Two of these studies indeed showed bright light was associated with benefit by every measure, but the statistical evidence was insufficient,[50] possibly because these studies needed more patients. The other was an unlucky study, in which, by chance, the patients who received bright light had a poorer prognosis at the outset than the patients with whom they were compared.[51]
A recent study of three-week light treatment of elderly outpatients was quite successful.[52] Dr. Klaus Martiny in Denmark has done an excellent five-week study showing that five weeks of light treatment was effective for nonseasonal depression.[53] Dr. Martiny has done an eight-week study combining light, wake therapy and antidepressant drugs which showed remarkable benefit.[54]
In summary, there is now extensive evidence that bright light treatment reduces symptoms for both nonseasonal and seasonal depression. For nonseasonal depression, the triple combination of bright light, half-night’s wake therapy, and medication might produce approximately a 35% reduction in symptoms in one week. There is a need for longer-term studies of the triple therapies. The good news is that with the new studies and new developments in light treatment, we may now be quite sure that we can improve the treatment of depression.
Additional
sources of information on light treatment
Society for Light Treatment
& Biological Rhythms, www.sltbr.org![]()
![]()
Center for Environmental Therapeutics, www.cet.org![]()
![]()
University of British Columbia Seasonal Affective Disorders Page, www.ubcsad.ca![]()
![]()
Bright Light for Depression: The Scientific Evidence
Bright light treatment for winter depression has been supported by dozens of studies demonstrating beneficial results (though there have been a few studies with unsuccessful results).[55] The Clinical Practice Guidelines issued by the U.S. Department of Health and Human Services[56] recognized bright light as a generally accepted treatment for winter depression.
Regarding the more-common non-seasonal depression, a formal Cochrane Collaboration meta-analysis showed that bright light is effective for non-seasonal depression.[57] Cochrane reviews are the international gold standard for evaluating the clinical evidence for various treatments. In an abstract, Tuunainen expanded this analysis. A formal American Psychiatric Association Review found that bright light was effective for SAD but questioned the value for non-seasonal depression.[58] However, the Psychiatric Association authors later admitted that they had made an error in computing their meta-analysis, so the benefit was greater than they had concluded. A more recent French review concluded that bright light therapy was useful for nonseasonal depression, at least combined with antidepressant drugs.[59] There have now been several independent systematic reviews concluding that light treatment is effective for nonseasonal depression.[60]
Recent studies emphasize the usefulness of bright light in treating depressed elderly individuals in the home[61] and in treating pregnant and postpartum women with depression.[62] Interest has been renewed in “chronotherapeutics,” a combination of morning bright light treatment with wake therapy, sometimes combined with moving the sleep interval a bit earlier as well.[63] As of 2019, I do not know of adequate randomized comparisons of the effectiveness of combined chronotherapy versus morning light treatment by itself, but the combined benefits of chronotherapy do appear rather encouraging.
5.A. Is bright light only good in winter?
The earliest controlled report of bright light treatment for seasonal affective disorder (SAD) described remarkable 52% net benefits within one week; however, the bright light–treated patients were given high expectations which were not matched in the placebo-treated group.[64] Patients with high expectations often report improvement through the power of positive thinking, but benefits of positive thinking need to be separated scientifically from the effects of bright light. Later and larger studies of SAD treatment have indicated that bright light may not be more useful than antidepressant drugs or psychotherapy.[65] It does not afford a direct randomized comparison, but bright light for non-seasonal depression did better compared to fluoxetine than did bright light compared to fluoxetine for SAD in somewhat similar studies both carried out by Lam and colleagues.[66]
Even if we were sure that SAD patients responded better to light than other depressed patients, it would often be hard to tell what type of depression a person suffers. Follow-up of SAD patients by Dr. Rosenthal’s research group showed that the majority of patients first defined as SAD eventually displayed summer symptoms, if their illnesses continued to recur, and many needed antidepressant drugs.[67] Over follow-up, such patients may be perceived as nonseasonal according to accepted criteria. Many SAD patients eventually require both bright light treatment and antidepressant medications outside the winter months. Because of controversial criteria and complex clinical course, it may often be impossible to define whether a depressed patient does or does not have SAD, so restricting light therapy to SAD would not be very practical.
To summarize my opinion, even when seasonal pattern can be distinguished, there is no assurance that light treatment will work better in seasonal than in nonseasonal patients, nor does seasonality exclude the usefulness of antidepressant medication in addition to bright light. In conclusion, in my opinion, bright light is useful for people who are depressed, whether or not we think that they have SAD or winter depression. It is likely that for both nonseasonal and SAD patients, a combination of bright light and antidepressant drugs is advisable, with possible addition of wake therapy and psychotherapy.
5.B. More perspective on antidepressant medication
To have perspective on the values of bright light treatment, it is useful to critically consider the benefits which result from antidepressant drugs. Hundreds or perhaps thousands of controlled trials of antidepressant medications have been reported, with a great preponderance of evidence that medicated patients improve somewhat faster than comparison patients given placebo. Placebo means an inactive, dummy treatment. Nevertheless, perhaps misled by pharmaceutical company marketing, many physicians suppose that the benefits of antidepressant drugs are greater than such trials actually demonstrate. The benefits were generally minor on average.
Because antidepressant medications may require six to 16 weeks to achieve substantial benefit, patients given placebo (dummy pills) for the same interval often display spontaneous remission. They get better by themselves, perhaps helped by hope and by encouragement from the researchers. The alleviation of symptoms attained during antidepressant drug treatment in most studies is due more to this spontaneous remission than to medication benefits. The benefits of antidepressant drugs are only clearly understood when the percentage remission of symptoms achieved with placebo is subtracted from the remission accompanying medication.
Only recently have overall and unbiased assessments of antidepressant drug effects become available. A compendium of antidepressant drug trials in thousands of patients reported to the U.S. Food and Drug Administration provided a general summary of antidepressant drug effects.[68] The advantage of this report over previous compendia was the inclusion of rather unsuccessful studies which the pharmaceutical manufacturers were obliged to report to the FDA, though they may not have wished to see such results published. In these studies, the eight-week net benefit of antidepressant drugs on the Hamilton Depression Rating Scale was only 8–12% better than the result with placebo. Another analysis of some of the same data found that the placebo groups had improved 58% percent at the last measurement and the drug-treated groups had improved 69%, a drug-related benefit of only 11%.[69] An analysis of fluoxetine results reached similar estimates, even though some of the authors were employees of the makers of Prozac.[70] Incidentally, this meta-analysis included only seven clinical trials comparing fluoxetine to placebo, whereas we have far more studies comparing bright light to placebo in nonseasonal depression. Dr. Lam’s study comparing fluoxetine with light treatment,[71] illustrated above, likewise had found representative antidepressant drug effects. A comprehensive meta-analysis using response criteria obtained rather similar estimates of antidepressant drug effects and also demonstrated that there has been a bias to publish more successful results and to leave less successful results unpublished.[72] Although these meta-analyses certainly demonstrated that antidepressant drugs have significant benefits for nonseasonal depression, the size of the antidepressant net benefit after eight weeks or more (approximately 8 to 19%) certainly does not appear superior to the one-week benefit of bright light treatment (approximately 12 to 35%). Moreover, very recent analyses have argued that antidepressant benefits are most impressive with the most severe depressions (e.g., those requiring hospitalization), whereas with relatively mild depressions, the benefits may be small or absent.[73]
It is worth noting that when antidepressant drugs fail to work well, addition of lithium treatment may be helpful. Also (particularly for young women), addition of thyroid hormone (T3 or triiodothyronine) may be helpful.
Although Dr. Lam’s studies did supply direct randomizing comparisons of bright light treatment approaches versus fluoxetine (a popular antidepressant, e.g., Prozac brand), most of the antidepressant drugs have not been directly contrasted with bright light, and the comparison trials have not been large enough and long enough to gain adequate perspective on the long-term benefits and risks. Although the benefits of bright light might be greater and are almost certainly more rapid than benefits of medication, much more is known about the long-term benefits of antidepressant drug treatment, which has been much more extensively studied when all drug studies are included. Moreover, there really is no reason to inquire whether one treatment of depression is better than the other. The important point is that bright light and antidepressant drugs are best used in combination, probably also combining at least a half-night of wake therapy and perhaps psychotherapy as well.
5.C. Be careful of dangerous new treatments for depression
In 2019, we have recently been reading considerable publicity about allegedly superior benefits for depression using implanted vagus-nerve stimulators or ketamine-related drug infusions. There has not yet been that much published about these new treatments, which have not been adequately studied. So far as I can understand, implanted vagus stimulators and ketamine infusions might be less effective than bright light treatments, probably far more dangerous, vastly more painful and inconvenient, and vastly more expensive. I have not seen evidence that these new treatments work more rapidly. The greater cost may be potentially profitable for some proponents advocating these two novel treatments, but I do not understand claims that the greater expense will help the patients more than bright light. Another kind of desperation treatment is deep brain electrical stimulation or lesioning.[74] I have not seen adequate evidence for these deep brain treatments, but decades of history of brain-lesioning treatments make me very suspicious of the safety of deep brain neurophysiologic approaches.
Remember, bright light treatment of depression has been tested in controlled-trials since 1981 and had previously been tried informally virtually throughout recorded history. There have now been dozens of randomized controlled trials published. Probably more than one million patients have tried modern bright light treatments for depression. Safety has been studied systematically, showing that serious risks of bright light treatment are evidently extremely rare. It would be misguided for a patient to try treatments that are obviously more risky without controlled trials evidence that the implantation or intravenous treatments give better results than bright light.

Advanced and Delayed Sleep Phase Treated With Bright Light
Let me explain about body clocks. We really do have 24-hour clocks inside our bodies. The main body clock is in the brain in a little area called the suprachiasmatic nucleus, smaller than a grain of rice. As the name implies, the suprachiasmatic nucleus lies in the hypothalamus just above (supra) to the optic chiasm – that is, above the place behind the eyes where the nerves from the eyes cross. The suprachiasmatic nucleus (SCN) receives nerve impulses from those optic nerves. Basically, bright light influences the suprachiasmatic nucleus clock to keep our bodies set to the correct body time. Of course, today, modern digital watches rarely need resetting, but our body clocks can run a bit too fast or too slow like mechanical watches did in the good old days. Thousands of years ago when humans were sleeping outside, the light of dawn probably set the suprachiasmatic nucleus each morning, something like how great grandfather used to set his pocket watch every morning by the time broadcast on the radio. The light just before sunset probably set our body clocks also, to keep them very nicely in time. If great grandfather’s watch was reset every day, running a little fast or slow never got to be much of a problem. If we are outdoors at dawn and sunset, our body clocks do not cause much problem either, because the light keeps the time set well enough.
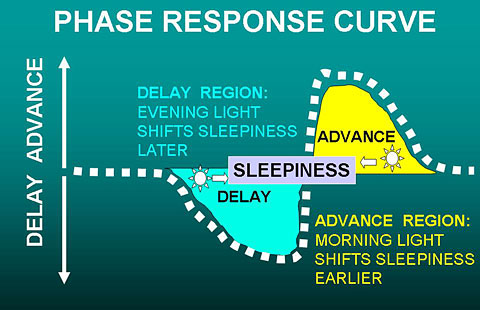
The figure above illustrates the human phase response curve.[75] When a person’s sleep has a normal relationship to the circadian clock system, light exposures from just before the time of falling asleep until past the middle of the night causes the body clock (and the nightly time of sleepiness) to delay later, as shown in light blue. Bright light in the last couple hours of sleep causes the clock (and the time of sleepiness) to advance – that is, to shift earlier, as shown in yellow. Light in the middle of the wake period, e.g., the afternoon sun, has little or no effect on the timing of the body clock.
This is exactly the same mechanism that sets the body clock in a rooster, so it knows when to crow in the morning. In fact, light sets the body clocks of the birds of the air like larks and owls and the beasts of the field, like cows and horses, lions and lambs. Light also sets the body clocks of flowers and trees. It is the natural way.
Our human body clocks do sometimes tend to run too fast or too slow, and if we are not outdoors at dawn and dusk for long enough, the timing of our body clocks can get to be a problem. In fact, there are two possible kinds of problem: the problem when the body clock is running too fast and the problem when the body clock is running too slow. Let us discuss each of these common problems.
6.A. Advanced sleep phase
When the body clock seems to run too fast, it gets ahead of the day, and sends its signals to the body too early. Then we say the timing of the body clock is advanced over what it should be (or the phase is advanced, to use a mathematical term). The main symptoms of advanced sleep phase are 1) falling asleep too early, and 2) waking up too early. People with an advanced sleep phase typically nod off in the evening reading or watching television – or even talking to the family. They may fall asleep before they go to bed. Sometimes they have to wake up to go to bed and turn off the light. Trouble paying attention to reading, homework, and favorite television shows is a problem for them in the evening. A more dangerous problem is falling asleep behind the wheel of a car in the evening. Later in the night, the person with advanced sleep phase wakes up too early. Their internal alarm clocks may wake them up at 3 am or 4 am or 5 am, long before the rooster crows, and they become distressed, because they would like to sleep later. For some folks, there isn’t much fun to be had at 4 in the morning, when everyone else is asleep.
Also, if the person with advanced sleep phase has somehow managed to stay up to a socially compatible bedtime, there may not be enough time before 3–5 am awakenings to get enough sleep. People with advanced sleep phase may typically feel most energetic in the morning and least energetic in the evening. Such a person is commonly called “a morning person” and displays “morningness” behavior.
To some extent advanced sleep phase arises from conflicts between social patterns and natural biology. Two hundred years ago, when most Americans lived on farms and there was little artificial lighting besides candles, it may have been customary to fall asleep at 8 or 9 pm and to awaken at 4 or 5 am to milk the cows, feed the chickens, and so forth. The life style of farm animals is in synchrony with the natural light cycle, so many animals get half of their sleep before midnight and have half of their waking hours before noon. People had somewhat similar habits. In a 21st century society, we like to stay up for prime time TV and The Late Show. Currently, many people do not start working before 9 am. In this social context, the sleep patterns of two hundred years ago may be perceived as a sleep disorder. Advanced sleep phase is often merely an inadaptability of natural biology to unnatural social customs.
Advanced sleep phase seems to be much more common as people live beyond 60 years of age into their 70s, and 80s. One theory for which there is some laboratory evidence is that our body clocks speed up as we age, even though most body processes are slowing down. A body clock which runs too fast tends to very gradually become advanced. Deterioration of vision may be a factor. As the lenses of our eyes become cloudy and thicken into cataracts, we see “as through a glass, darkly,” so that much less light strikes the retina of our eyes. With the eyes’ remarkable ability to adapt to changes in lighting, we may not realize the clouding of the lenses until they are shadowing almost 99% of the light falling on the corneas. Older eyes also have smaller pupils, which let in less light, like the higher f stops of a camera. Finally, glaucoma, macular degeneration and other retinal problems may impair the eyes’ light sensing mechanisms. All of these eye problems might cause elderly people to have a body clock poorly adjusted to afternoon-evening indoor lighting unless they receive extra light.
Advanced sleep phase seems to be more common among elderly women. We do not know why, but several studies have shown that among people of retirement age, the body clocks of U.S. women are set, on average, about an hour earlier than those of men. It is as if the internal alarm clocks of retired women are set to awaken them an hour earlier than those of their husbands. We do not know if this is a major factor which makes insomnia more common among elderly women, especially after menopause, but in most studies women have complained of insomnia much more than men do. A separate factor is though many doctors believe that the hot flashes and sleep disturbance of menopause go away after a few years, I think these symptoms often persist throughout the rest of life, unless the woman takes estrogen hormone replacement.
To inform our body clocks that sunset is undesirably early to become sleepy in our social organization, we must put enough evening light before our eyes for the body clock to react as if it were still day. Since rural electrification brought electric light to every home, it has become possible to light up our homes quite brightly long after the sun goes down. Lighting fixtures become more efficient year by year, so it is even easier to light up a home today than it was twenty or thirty years ago. The great enemy of good lighting seems to have become television. As the channels multiply, people watch more and more television or computer screens, which often are equally dim. Technologists tell us that a wedding of televisions, computers, and telephones is on the way, when life may be built around such screens. Because TV screens have not really been very bright, many people watch in rather dark rooms. Possibly, the larger, brighter TVs being sold in the last couple of years will help with this problem. In actual measurements of people from 60–79 years of age done over 20 years ago, we have found half of elderly people were spending the evening in less than 31 lux.[76] About 10% were spending the evening (probably watching television) in about 1 lux – about the same as sitting outdoors in moonlight! It is not hard to understand that the dim lighting of some TV rooms and living rooms is insufficient to make the body clock react as if it were day. Such dim evening light may result in an advanced sleep phase.
Solving advanced sleep phase is very simple for some people. Often, all that is needed is a brighter lamp by the TV chair. The most convenient lighting by a TV chair might be a fluorescent or LED column lamp or torchiere (a tall lamp like a torch).
In the past, I recommended a popular style of halogen-bulb “torchiere” lamp which bounces light indirectly off of a white ceiling and really lights up a room. Over 40 million of these halogen torchieres have been sold in the U.S. as the price kept coming down and down. There is no special advantage of the halogen lamps, except that they were extremely inexpensive and they have a fashionable appearance. Actually, the halogen lamps were inefficient for two reasons. First, halogen (and other) incandescent bulbs intrinsically use far more electricity than fluorescents of the same brightness. Fluorescents produce more light per watt. A 50-watt fluorescent and a 300-watt halogen are roughly equivalent. The halogen bulb produces a bigger electric bill. Second, the halogen’s very bright point of light and ultra-violet content might make it risky to look at 300-watt halogen light directly – something I never recommend. This is why the 300-watt halogen lamps are generally designed as indirect lighting. Because halogen torchiere light has to be bounced off the ceiling, indirect lighting is much less efficient than a fluorescent with diffuser that can be viewed directly. Another problem is that the 300-watt halogen bulbs get so hot that they can cause severe burns or set draperies or other objects which might touch them on fire. Over a hundred fires and several deaths have been reported due to halogen torchieres, but this is not a great risk considering over 40 million sold. Finally, the halogen bulbs burn out quickly and are difficult and somewhat expensive to replace.
Fortunately, fluorescent torchiere lamps are now widely available. A 50-watt fluorescent is roughly equivalent to a 300-watt halogen torchiere. The fluorescents will solve the safety problem and have superior energy efficiency. Fluorescent bulbs last much longer. LED lamps will have even better energy efficiency and longer life than fluorescents. Despite a higher initial cost, over several years, fluorescent and LED lamps will lower the electric bill enough to be less expensive in the long run. Because much of the torchiere light is indirect, a torchiere lamp may only produce 200–300 lux at eye level. For counteracting advanced sleep phase in the evening, a bluish-white “cool white” light is likely to work better than a “warm-white” light of the same electric consumption and brightness. That is, a cool-white or bluish-white bulb with “color temperature” rated above 5,000 K (even as much as 17,000 K) is likely to work better than one below 3,000 K.
The fluorescent light boxes which were discussed for treating depression can produce 10 to 30 times the lux at the eye as a torchiere of similar or greater wattage bouncing off the ceiling, because one can look directly at a light box placed close to the eyes. Nevertheless, torchiere lamps often seem to produce sufficient light for a TV room, a computer room, or other parts of the house. After all, 200–300 lux is about 10 times as much as the 31 lux which was our middle measurement of evening lighting for elderly people. I have seen several patients who have largely resolved a nagging advanced sleep phase problem with a simple torchiere lamp. There are probably many other ways of lighting a TV room that would work as well or better – I simply have not had as much experience with other lighting styles.
For advanced sleep phase, the time to use the right light is for 1–3 hours late in the evening, often when a person is sitting in a chair reading or watching TV (during dinner sometimes also works). It probably will not make much difference if a person gets up and down from the chair near the light, as long as the light is experienced much of the time. If a person does not stay in one room most of the evening, it may be necessary to brighten up more than one room. Some people need a longer exposure than others, depending both on the brightness of the lighting and on individual factors. The later in the evening that the bright light is used, the more powerful will be its benefit for advanced sleep phase. However, some people will find that they should dim down their lighting for about one hour before they wish to go to bed, to avoid overdosing and causing trouble with falling asleep.
A person with advanced sleep phase might begin to feel some benefit after using brighter evening light every night for a week, but it might take a month or two before the maximum benefit is reached, especially because it takes some time to restore good sleep habits. This treatment does not work unless the evening light is turned on at full brightness: I advise against using dimmers. Once the problem is under control and the body clock has readjusted, a person with advanced sleep phase can often afford to skip bright evening light on special evenings when they entertain or go out. Nevertheless, usage of brighter light in the evening probably needs to become a life-long habit. A person who benefits from bright evening light will often relapse within a month after skipping the bright light too often.
An interesting problem with bright evening light occurs when a spouse or other housemate has a different sort of body clock, possibly even a delayed sleep phase (see below). Bright evening light which is good for one person may be too much for another. This can usually be adjusted simply by arranging the placement of the lighting within the room, so that the person needing the bright light is in a brighter area than the person who does not need it. Couples have told me, however, that treating one spouse sometimes helps the other also! It all depends on the ways in which people are similar or different.
People with advanced sleep phase should avoid very bright light early in the morning, because morning light has a harmful effect for people whose body clock is already too advanced. Sometimes, walking or running outdoors soon after dawn or a long drive to work in the morning is a problem making advanced sleep phase worse. A person with advanced sleep phase might be wise to wear blue-blocking sunglasses when outdoors between the time when the sun comes up and noon. Such sunglasses have a particular orange color which filters out the blue light that is most likely to cause phase advance.
6.B. Advanced sleep phase and depression
There are two conditions which typically cause early awakening: advanced sleep phase and endogenous depression. “Endogenous” depression means the kind of melancholic mood which seems to come from inside the body and less from psychological stresses. There seems to be some relationship between advanced sleep phase and depression, particularly in middle age and beyond (though there are also many depressed people who are delayed). Some of my patients with advanced sleep phase problems likewise also seem a bit depressed, so it is difficult to distinguish the two conditions. Bright light in the evening seems to work both for advanced sleep phase and for depression with early awakening, so sometimes it may not be too important to distinguish which condition a person might have (or perhaps a person suffers both).
Nevertheless, if a depression is serious enough to keep you from your normal occupations and pleasures or to cause weight loss, guilt, thoughts of death, or other serious distress, let me repeat that you should talk it over with your doctor. For serious depressions, light treatment should often be combined with the treatments like anti-depressant drugs and counseling. Lithium may have some beneficial effect for advanced sleep phase. Moreover, for more serious depression, I often prefer one of the powerful fluorescent or LED light boxes to the torchiere lamps, since the torchiere lamps simply do not deliver as much light to the eyes. If a simple light treatment is not enough for a serious depression, it is definitely time to talk with your doctor.
6.C. Delayed sleep phase
When the body clock seems to run too slow, it gets behind, and sends its signals to the body too late. Then we say the timing of the body clock is delayed past what it should be. The phase is delayed, to use the mathematical term. The symptoms of delayed sleep phase are 1) falling asleep too late, sometimes after lying in bed awake for many hours, and 2) waking up too late and having trouble getting up on time. People with delayed sleep phase typically have trouble falling asleep unless they stay up much later than they would wish to. Having gone to sleep so late, people with delayed sleep phase often oversleep and have trouble getting to work or carrying out morning activities, as if their bodies’ internal alarm clocks do not ring on time. Indeed, people with severe delayed sleep phase will sometimes sleep past noon. People with delayed sleep phase – unless they drag themselves out of bed – are often rather long sleepers, and they often have a grumpy mood or real depression.
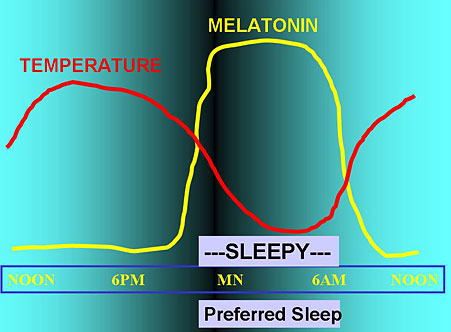
In the figure above, a normal person has the “sleepy” phase of their body clock aligned with the interval when they prefer to sleep, so they sleep well. Blood melatonin begins to rise an hour or two before sleepiness develops, and melatonin falls at about the time of awakening. Body temperature falls in the evening and during sleep, beginning to rise a couple of hours before awakening.
In the figure below, a person with delayed sleep phase disorder finds that the time of sleepiness does not begin until much after the time of preferred sleep onset, but sleepiness persists after the person would like to be able to get up for the day. The physiologic rhythms of melatonin and body temperature are also delayed, making it hard for the delayed person to arise at the preferred time.
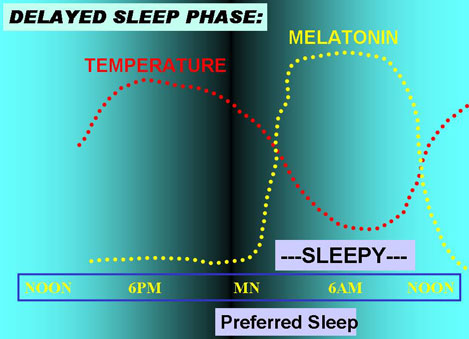
Of course, when people prefer to sleep depends on school and work schedules and many social factors, and the timing of their sleepiness varies also.
People with a delayed sleep phase often feel somewhat rebellious or angry with authorities, perhaps because they have experienced so many years of people insisting that they wake up when their body clocks are telling them to keep on sleeping. Unfortunately, people who do not come to school or work on time are often regarded as lazy, so they have not received the sympathy they deserve for their body clock problems. Also, since people with delayed sleep phase may not feel very alert until well past noon, and their best and most energetic hours are sometimes past midnight, they may have learned to enjoy their habitual late activities and be reluctant to give them up for bed. Successful treatment needs a willingness to change customary habits.
The timing of sleep patterns – being advanced or delayed – does run in some families. There is evidence that people with delayed sleep phase have some genetic changes in the body clock. It is also peculiar that delayed sleep phase seems to develop somewhat late in puberty – often around 16 to 18 years of age – and be at its worst in the early 20s. College students and graduate students without fixed classes seem to be particularly prone to delayed sleep phase – there certainly isn’t much quiet in the dormitories before midnight at our university. One wonders if that rebellious trait – the wish to get out from under the thumb of authority – sometimes contributes to a delayed sleep phase. There is even some evidence in animal studies that the younger adult animals adopt a different daily activity rhythm, apparently to keep out of the way of the more dominant more mature adults. Nevertheless, we do see delayed sleep phase among mature adults and even in some elderly people.
It is apparent that too little morning light exposure has something to do with the development of delayed sleep phase. Because dawn is later in winter, we all get up later in winter because standard time causes us to set our alarm clocks an hour later than in summer daylight savings time. Of course, the dawn is earlier in the summer. A number of studies indicate that even after taking account of the time change, people tend to stay up later by the clock and get up later in winter than in summer. This trend seems to be especially prominent in northern areas (above 45° latitude), where winter nights are particularly long. In those areas, people may see no bright daylight in the morning, as they arrive at school or work before the sun comes up. Theorists have speculated that experiencing dawn is particularly important for setting our body clocks, and even, that the gradually waxing light of dawn has some special signaling significance for the body clock. In fact, MS Stephanie Rosen in my laboratory found some evidence that people who have thinner-lighter window shades (that let in more dawn light) tend to fall asleep a little more rapidly and arise a little earlier.
Whether or not the waxing light of dawn is an important signal, it is a fair bet that people whose sleep phase is delayed are not experiencing enough bright light in the morning. That is the key to treatment.
The best treatment for delayed sleep phase is to increase the dose of light that the person receives soon after their habitual awakening time. The brighter the light, the sooner after usual waking up it is experienced, and the longer the period of exposure (up to 3–4 hours), the better the result is likely to be. The problem is that delayed sleep phase is often a stubborn condition that can only be controlled by very bright light for 1–2 hours each morning. Arranging to receive that light may be hard to fit in with daily habits. I usually find that people with delayed sleep phase need one of the bright fluorescent light boxes. Although torchiere lamps and other increased lighting can be helpful, ordinary fixtures usually do not seem to be sufficient. One convenient way to get a strong dose of morning light is to use a light box (maybe a box arranged for 10,000 lux) for 30 min at breakfast time, since eating and reading the morning paper do not interfere with the benefit. For people who work at a desk, placing the light box on the desk and turning it on all morning might be effective, even if one cannot sit at the desk all of the time. If it is convenient to be exposed to bright light for several hours each morning, around 2,000 lux might well be sufficient, allowing the light box to be placed at the far side of the desk, or allowing the use of a more customary-appearing bright fluorescent or LED desk lamp.
Looking at the phase-response curve (below), we see that the best time to give bright light to somebody with delayed sleep phase is as soon after their spontaneous waking time as possible, that is, just when their natural sleepiness ends. This is a bit complicated, since at the beginning of treatment, the body's preferred waking time may be quite late in the day. It is probably best to start using the bright light after the (rather late) spontaneous waking time, and then to give the treatment earlier and earlier in the day as the person starts falling asleep earlier and waking up earlier. A really strong dose is best for the first few days of treatment to reset the body clock, so I often advise that patients start treatment on a weekend when it is practical to spend 3–4 hours outdoors right after waking up. Once a person is able to fall asleep at a reasonable hour and to awaken at the desired time (e.g., 7 am), the best time for treatment is in the early morning. In the first week or two of correcting delayed sleep phase, it is very important to use bright light treatment for a full dose every day, seven days per week.
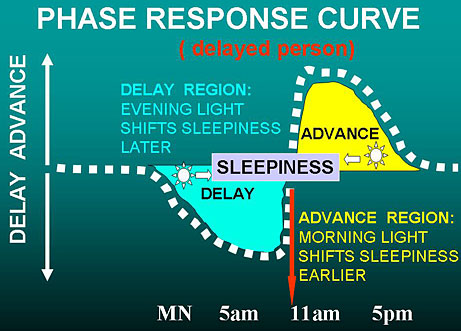
As diagrammed above, a person with a delayed sleep phase usually also has the phase response curve delayed, and the end of the natural sleepiness time is late in the morning or even after noon. We are talking about when it is easiest biologically to sleep and then arise (e.g., on weekends), not when the person needs to arise to get to work on time. Because the body clock and its phase response curve are delayed, the best time for light to advance the body clock is also later. Moreover, as shown above, bright light early in the morning might make the delay worse. This can be a problem for delayed people who struggle to get up early to get to school or work, when the person’s phase response is still in the delay zone. For such occasions, blue-blocking orange sunglasses may be helpful outdoors to prevent light exposure on the way to work from making things worse. Once the delay in the body clock is corrected, the phase response curve will be advanced and early morning light will be helpful.
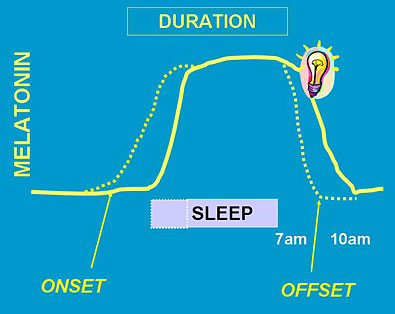
The diagram above shows how bright morning light pushes melatonin onset and offset earlier (dotted lines), so the person can get to sleep earlier.
Just as it may be hard to set an alarm clock for the proper time but easier to set the alarm to ring daily once it is set to the correct time, similarly, it takes less bright light to keep the body clock set properly, once a delayed body clock has been reset. After a delayed body clock has been successfully readjusted and the person’s habits have readjusted to the new sleep hours also, a bit less effort may be needed to keep the body clock from delaying again. Nevertheless, people with delayed sleep phase commonly relapse if they stop using light treatment loyally. Also, it is very harmful for people with delayed sleep phase to stay up late on weekend nights and to sleep late on weekends and days off. A person with delayed sleep phase should try to keep a regular wake-up time, seven days per week, because once a little relapse is permitted on days off, the person with delayed sleep phase will find it too hard to recover.
There are many ways of arranging to get added bright light in the morning, such as installing bright lighting in the bathtub or around the bathroom mirror (like the dressing-room lights of movie stars), increasing lighting in the bedroom and kitchen, and removing sunglasses when driving or walking to work. Unfortunately, in my experience, these arrangements are often insufficient for a seriously-delayed sleep phase. Difficult delayed sleep phase usually requires a fluorescent or LED light box. Spending 30–60 minutes or more outdoors in early morning daylight (after the sun comes up) should be effective. Unfortunately, winter fog and rain often make getting daylight exposures difficult even in San Diego (where I live), whereas in the coldest and hottest parts of America, getting enough morning outdoor daylight is well-nigh impossible during parts of the year. Do not depend on sitting near a window or opening curtains – it is almost never bright enough. For these reasons, I do recommend the bright light boxes for delayed sleep phase.
The theoretical importance of the dawn signal has inspired some doctors to try “dawn simulators,” which slowly increase artificial room lighting in about the same pattern that dawn might creep through a bedroom window. These doctors believe that the natural dawn signal is so powerful that it will reset the body clock even during sleep, when the light has to pass through the eyelids, and that dawn simulation does not have to be very bright. Several dawn simulators designed to mimic the light of dawn are now being sold, though they have not been tested very well. There is preliminary evidence that dawn simulators may have some benefit, although perhaps not as powerful a benefit as a 10,000-lux light box. In treating patients with SAD who tend to get up late, lighting waxing only up to 250 lux, entering through closed eyelids during sleep, did seem to reset the body clock and to partially relieve the depression.[77] Another test of administering increasing brightness through a sleep mask seemed to show some benefit.[78] It would be nice to see dawn simulators more thoroughly tested, since they may be a particularly convenient way of dealing with delayed sleep phase.
Some Japanese researchers have reported that supplemental vitamin B12 is useful for delayed sleep phase, even when the patient does not have any evidence of vitamin deficiency by the usual criteria. They recommend about 1-2 mg. (1,000µ or 1,000-2,000 micrograms) of oral vitamin B12 daily. This is much more than the minimum daily requirement which is contained in most multivitamin pills. The vitamin B12 which can be easily purchased in 1 mg. doses at North American grocery stores is a slightly different vitamin from that tested by the Japanese, but it probably makes no difference. Unfortunately, the best Japanese test of vitamin B12 for delayed sleep phase did not demonstrate any good effect. Nevertheless, since vitamin B12 in high doses has practically no known side effects and is very inexpensive, I do recommend that people with delayed sleep phase try the 1 mg dosage.
6.D. Depression and delayed sleep phase
Depression does seem to be associated with delayed sleep phase, particularly among young adults and women before menopause, and particularly when the problem occurs in the winter. Indeed, delayed sleep phase disorder and seasonal affective disorder tend to be associated (that is, comorbid). Our research group also gathered some evidence that some of the same genetic variations may cause delayed sleep phase and depression, and this has been supported by large population genetic surveys. [79] With delayed sleep phase (as with advanced sleep phase, as previously mentioned), it is often difficult to tell when the problem is a sleep timing problem and when it is a real depression, because the problems often seem mixed together. Bright light which corrects delayed sleep phase does usually seem to lift mood symptoms also. Nevertheless, as I mentioned before, if a depression is serious enough to keep you from your normal occupations and pleasures or to cause weight loss, guilt, thoughts of death, or other serious distress, let me repeat that you should talk it over with your doctor. If light treatment for delayed sleep phase does not alleviate the depressive symptoms, it is certainly time to talk with your doctor.
6.E. Melatonin and delayed sleep phase or advanced sleep phase
Melatonin is a night-signaling hormone. It is generally higher at night both among humans (and other creatures) that sleep at night, and also higher at night among rodents and other creatures that are awake and active at night and that sleep in the day. Obviously, melatonin is not primarily a sleep-inducing hormone. Melatonin has a role in coordinating circadian rhythms throughout the brain and the rest of the body, even impacting rhythms that peak at different times. As mentioned, the evening rise and morning fall of melatonin are late among “evening people” with delayed sleep phases. Probably a delayed body clock and delayed sleep tend to delay melatonin and likewise, a delayed melatonin pattern tends to delay sleep and the body clock. Conversely, the evening rise and morning fall of melatonin are early among “morning people” with advanced sleep phases. Some melatonin effects on hormone systems and mood are discussed in Chapter 9.
Taken at bedtime, melatonin has little effect in shortening time to fall asleep, though it accelerates sleep onset when taken an hour or two before bedtime. When taken by mouth, ordinary melatonin is mostly metabolized in an hour or two. As a consequence, melatonin is of little or no use for increasing total sleep at night, except among those evening people having problems with delayed sleep phase. Melatonin in very low doses (e.g., 50-500 micrograms) might be potentially useful for chronic delayed sleep phases. An extended release form of melatonin (brand name Circadin) is licensed as a prescription sleeping pill in Europe (not in the U.S. as of 2019). Tests of Circadin sponsored by its manufacturer demonstrated some usefulness and a favorable side-effect profile, but evidently the U.S. Food and Drug Administration has been skeptical of Circadin and has not licensed it. One might speculate there could have been safety concerns.
Although as much as 5% of the U.S. population has been reported to be taking melatonin, I know of very little long-term population safety data and no long-term safety trials. In my own data, although not statistically reliable, there was a trend for women with higher melatonin secretion to have shorter lives. Much larger studies are needed. It is possible that melatonin may have anti-cancer properties when taken routinely, but it is also possible that melatonin suppresses sex hormones and promotes depression.

Side Effects of Bright Light
They say that everything good is either risky, immoral, or fattening. Light treatment is neither immoral nor fattening, but unfortunately, it does have risks that you should know about. To put this in perspective, water has risks, sugar has risks, salt has risks, apples and oranges and sirloin steak have risks, sunlight has risks, and artificial light treatments have risks also. It takes some judgment to know how much is too much – of water, sugar, salt, or indeed, of light.
7.A. The risk of mania
All effective antidepressant treatments, including bright light, can trigger mania. Manias triggered by bright light can be serious, and perhaps constitute the most important risk of bright light treatment.
What is mania? Mania is a specific unusual mood in which a person becomes too happy, too euphoric, too irritable or too hyper, in a way which causes trouble. Manic people suffer from rapid speech, they talk too much (they feel pressure to keep speaking), and they have too many ideas, causing difficulty concentrating. They are distractible and often jump from one idea to another. They are hyperactive, and often awaken early or cannot sleep. A person who is manic is not the person’s usual self. Sometimes manics venture into things with a high probability of getting hurt physically or socially or suffering financial losses.
Although mania may resemble happiness, cheerfulness, or high energy, in its extreme form, mania is quite risky for the manic person and for the people around. Let me give you some examples of the poor judgment manics show. A manic patient was driving 80 mph down the freeway, and when stopped by a highway patrol officer, he started a fight. He was lucky that the patrolman only beat him up a little. Another patient, a conservative middle-aged mother of several children, became manic enough to go down to the red-light district and solicit male customers. An impoverished patient bought two Cadillacs in one day, though he couldn’t afford a new car at all. Another manic patient on pension ordered a private jet, asking the company to paint it custom yellow for him. A manic patient left his wife and drove a thousand miles, got up in the middle of the night, took off all his clothes and ran around a motel parking lot. A manic patient threatened the life of the President, so the Secret Service considered arresting him. You wouldn’t want all the trouble that mania causes for people and their families.
Mania occurs in people with bipolar disorder, another name for what we used to call manic-depressive illness. The distinguishing feature of bipolar disorder is that a person with this disorder has at least once suffered from mania or at least mild mania (what we call hypomania). Fortunately, I have never heard of severe manic symptoms being triggered by bright light in a person who had not previously suffered from mania. The risk seems to be very low for people who have never had mania. People with bipolar disorder commonly experience periods of depression, when an antidepressant treatment such as bright light might be needed. Indeed, they may suffer more from long depressions than from briefer manias. Bipolar disorder seems to be a biological and genetic illness, just like diabetes, with the peculiar feature that the illness seems to recur and recover, sometimes with little obvious pattern.
When somebody with bipolar disorder is treated with bright light, sudden mania might occur. I know of a patient with bipolar disorder who injured a hospital staff member and needed to be placed in restraints within a few hours after a bright light treatment. Fortunately, this severe kind of reaction to bright light is uncommon except among people with bipolar disorder who have had at least one period of mania in the past, and it seems to be rare if the person is taking a mood stabilizer such as lithium, carbamazapine (Tegretol), or divalproax (Depakote). Most people with bipolar disorder should be taking such a mood stabilizer. Some recent studies suggest that the risk of mania may be no greater with light treatment than with other effective antidepressant treatments, or even less.[80] Perhaps the risk of mania with light treatment is additional evidence that light treatment can be antidepressant. Nevertheless, if I had ever had a mania, I do not think I would risk bright light treatment unless I were taking a mood stabilizer, and unless I were under close supervision by a doctor.
It is likely that wake therapy also increases the risk of mania.
Mild manic symptoms or irritability have been triggered by bright light in seemingly normal research volunteers and among people who have never had mania. Usually the problem is just poor sleep or feeling a bit angry or feeling a bit hyper. Nevertheless, it is important to recognize these symptoms when bright light produces them, because the dosage of bright light should be immediately reduced or the use of bright light should be discontinued until these symptoms go away. Some people find that they must balance their dosage of bright light: too little light leaves them depressed, but too much may leave them irritable or hyper. Certainly, anybody who is having these symptoms from bright light should immediately discuss them with a doctor.
There is some indication that the risk of mania is greater when bright light is used in the early morning. Possibly, waking up early increases the risk of mania, or possibly the risk comes when the body clock is advanced too early.[81] Researchers at the National Institute of Mental Health have reported preliminary studies which suggest that when bipolar patients experience switches between mania and depression at least four times a year, bright light treatment is safest in the mid-afternoon.[82]
7.B. Sunburn and skin cancer
Much as we love the sun, we all know how sunburn hurts. More serious, sunburn and too much sun cause skin cancers, some of which can be fatal. The risk of sunburn and skin cancers such as melanoma seems to be increasing, because air pollution is reducing the layer of atmospheric ozone which normally shields us from most of the sun’s ultraviolet rays. Damage to the ozone layer is allowing the sun to cause more sunburn than sunshine used to cause. People need to get bright light without increasing their risk of sunburn.
Fortunately, you can get plenty of light without sunburn. The benefits of light for depression, the body clock, and sleep, seem to come through the eyes. For good sleep and good mood, there is no need for any sun at all to fall on the skin. From my point of view, long sleeves, long pants, and a hat are just fine for people who want to get their bright light outdoors. Sunscreen may help. There is no persuasive evidence that light hitting the skin is antidepressant.
I have also explained that bright light in the early morning or just before sundown is often the best for the body clock. From the moment the sun rises above the horizon (at least if it is a clear day), the light may be bright enough to do you some good and keep you from wilting. The morning and before-sunset evening times are therefore particularly good times to get outdoors in daylight, possibly even more effective than mid-day for most people, and these times soon after dawn and shortly before sunset give the safest daylight for the skin. Unfortunately, the minute the sun goes below the horizon, the twilight grows too dim to be useful for mood. Oddly enough, the ultraviolet rays which cause sunburn are scattered more by the atmosphere and absorbed more by ozone than are the visible colors of light which make up sunlight. As a consequence, the strong ultraviolet which causes sunburn is mainly a problem when the sun is almost overhead. The greatest risk of sunburn is between 10 am and 3 pm. There is less risk of sunburn before 10 am or after 3 pm. For these reasons, I usually recommend that people try to get most their daylight exposures before 10 am or after 3 pm, except in the winter, if the sun is low even near noon. The risk of sunburn is less important, of course, for those using long sleeves and a hat or sunscreen for protection.
Except in winter, if you would like to get your daylight exposure at mid-day, consider sitting in the shade. Since it is light entering the eyes that is important for your mood, not what falls upon your skin, your eyes can usually be directed towards a sunny part of the environment even when you are sitting in the shade. Also, in most sunny weather (except very dark rainforests), even shade is several thousand lux during mid-day, and therefore the light is helpful.
Most artificial lighting does not contain enough ultraviolet rays to create any risk of bright light treatment, but there are exceptions. Some “full spectrum” bulbs can cause a sun burn if you get very close and if the light does not have a diffuser which filters out the ultraviolet. There is also some ultraviolet produced by the halogen bulbs, but I doubt that much is reflected in the indirect lighting. Purple ultraviolet tanning lights, of course, give off intense ultraviolet light, so you should not look at that light. Some LED lights also give off considerable ultraviolet unless the ultraviolet is shielded.
7.C. Eye burn
It is true that you can burn the retinas of your eyes by staring at the sun. You should not stare at anything that bright, whether the sun itself or any very bright point of light. As I have mentioned, fluorescents with diffusers spread the light out enough to minimize this risk. Using indirect lighting also eliminates this risk by spreading out the very bright point of light. So far as I know, you can’t do your eyes permanent harm with any of the commercial fluorescent lights or with incandescent lighting used indirectly. It is worth a reminder, nevertheless, that you should not stare at anything so bright that it hurts your eyes. The limit of brightness above which the risks outweigh the benefits is probably around 10,000 lux. Anything much brighter than 10,000 lux is probably unwise. People with special eye problems should ask their eye doctors for further advice about their special problems.
Some doctors have theorized that people taking certain drugs such as major tranquilizers (example: Thorazine) or lithium could hurt their retinas with bright light treatment. Since millions of people have taken these drugs and have gone out into sunlight, I doubt that this risk is more than minor.
There is a kind of light damage to the eyes which might be caused by the ultraviolet rays in ordinary sunlight. It seems that some clouding of the lens and cataracts may be increased by very extensive exposures to the ultraviolet light in outdoor sunshine – the kind of exposure which fishermen experience if they are out on the water every day for much of a lifetime. It seems unlikely that the kind of daylight exposures that I have recommended (only an hour or two a day over the long run) would have any measurable effect on the lenses of the eyes. However, concern about cataract might be another consideration for trying to spend your time outdoors primarily before 10 am or after 3 pm, since most of the ultraviolet reaches us near mid-day.
7.D. Sleep disturbance risks
With light as with other treatments, there can be too much of a good thing. As we have discussed, bright morning light tends to make us fall asleep earlier and awaken earlier. Thus, bright morning light is the treatment for delayed sleep phase. Conversely, too much morning light can cause the opposite: an unpleasant degree of advanced sleep phase and early awakening. Similarly, although bright evening light is a treatment for advanced sleep phase, too much bright evening light can cause trouble falling asleep and trouble waking up in the morning. Some scientists also think that bright light close to bedtime prevents melatonin from increasing in our blood, as it usually does at that time, and that this may cause trouble with falling asleep. A person using artificial bright light may need to experiment with the timing, duration, and brightness of bright light if sleep problems of these types develop.
7.E. Headache and eye strain
Some people using artificial bright light treatments have reported temporary headaches or eye strain caused by the light. These symptoms do not seem to be serious or to indicate any permanent injury, but they certainly can be unpleasant. If fluorescent light is being used with 60 cycle flicker, an electronic high-frequency ballast will probably reduce the risk of eye strain. Most people try to reduce the intensity or duration of the light treatment to reduce these symptoms, unless they find that the benefits of the light are greater than the symptoms caused.
7.F. Suicidal thoughts
In the great majority of cases, bright light treatment (especially in the morning) lifts a person’s mood and increases the person’s energy. Occasionally, however, the effect of antidepressants such as bright light upon a depressed-exhausted person may be to increase energy in a harmful way. There are a couple of cases reported where bright light treatment led to increased suicidal thinking, and at least one suicide has been reported. If the result of bright light treatment is to increase suicidal thinking, it is time to stop the light and time to see a doctor that very same day.
7.G. Other risks of light
Some other milder side effects of bright light treatment have been reported, but these seem less serious, and I am not certain if they are real. Besides headache and eye strain, nausea, diarrhea, and increased sleep are sometimes associated with bright light treatment. Migraine may be triggered.
Good Sleep Habits
Since much of this book has been about using bright light to sleep better, it may surprise you that I think many people try to sleep too much. We are all familiar with the unpleasant feeling of having slept too little, but many of us have not thought about the possible harm of trying to sleep too much.
You may have heard somewhere that eight hours of sleep per night is recommended for optimal health. I do not agree with recommending eight hours or more of sleep for adults. In our studies in San Diego, the average adult is actually asleep only between 6 and 6.5 hours a night. Moreover, The Cancer Prevention Study II showed that people who report sleep of 6.5 to 7.5 hours live a bit longer than people who report sleep of eight hours or more.[83] The shorter sleepers lived longer! Even some people who slept as little as 3.5 hours lived longer than those who slept eight hours or more. Certainly, if you get only 6.5 or 7 hours of sleep a night and are not too sleepy in the day, you are probably sleeping enough. A recent systematic review found that long sleep was significantly associated with cardiovascular mortality but short sleep was not.[84] Another recent paper found that sleep of eight hours or more predicts future Alzheimer’s Disease.[85] My opinion of the healthiest sleep duration is based on my own studies of data from over two million research participants. Additional studies with further millions of participants have confirmed my viewpoint. If somebody claims to have evidence that you need eight hours sleep for health, ask them how many million volunteers they have studied.
Incidentally, when we record sleep in people above age 60, the amount of brain wave sleep is often about an hour less than the person reports on a questionnaire. In a study of elderly volunteers for the Women’s Health Initiative, we found that women whose recorded sleep was 5 to 6.5 hours lived the longest.[86]
Studies show that in the range that most Americans sleep (which is reported to be six, seven, or eight hours or so), there are few discernable differences between people. This may surprise you, but people who sleep six hours seem to be about as happy as people who sleep eight hours or more. Moreover, people who sleep six hours get just as much work done and are more likely to be employed than people who sleep eight hours or more. There may be some tendency for people with the shortest sleep times (five or six hours) to be outgoing and energetic, whereas people with the longest sleep times (nine or ten hours) seem to be more introverted, more imaginative, and (on average) more depressed. Notice the surprise! People who sleep a bit less than average may be less depressed!
Indeed, hospital studies of depressed patients show something very surprising. When depressed patients are kept awake all night (or at least for the second half of the night, e.g., after 2 am), they surprisingly feel less depressed the following day. The sleep loss helps depressed mood. This was part of the wake treatment which is now a part of chronotherapeutics and the triple treatment of depression. Moreover, after the wake therapy, taking a nap makes depressive symptoms recur. Wake therapy would be a very popular treatment for depression except for one problem: people with depression who stay up during the night do get sleepy, and after they sleep soundly the next night, the low mood usually relapses (unless bright light is used). Evidently, although it is true that people who are getting depressed have poor sleep, it is not true that getting more sleep helps depression. Often it is quite the opposite.
For these reasons, most depressed people should not struggle to get more sleep. People may often improve their moods by getting up a bit earlier.
There is another factor. Spending more time than necessary in bed – as you might expect – causes people trouble with falling asleep and makes them more likely to awaken while in bed. Sometimes, the frustration of lying in bed awake adds to the problem, and it builds on itself, getting worse and worse. The more time the person spends in bed trying to get more sleep, the more trouble develops in falling asleep and the more the person awakens in the night. Surprisingly, it seems that spending too long in bed might be a major cause of sleep trouble among both elderly and depressed people. Fortunately, there is an easy solution.
People who are spending a lot of time in bed lying awake should spend less time in bed. This means either going to bed later or getting up earlier. Getting up by a regular time seems to be important, so trouble falling asleep should not persuade you to sleep late. The less time you spend in bed, the sleepier you will be the next evening. Think about it. If you spend less time in bed, you will surely tend to fall asleep more easily and sleep more soundly in the future. Moreover, the less time you spend in bed, the more you will gradually restore the habit of falling asleep quickly after going to bed, and the more you improve the habit of sleeping soundly. Some doctors would recommend that you should not spend more time in bed than you actually sleep. If you think you only sleep as little as six hours a night, perhaps you should spend only six hours in bed until you are sleeping all six hours. Then you can try increasing time-in-bed about 15 min., e.g., to six hours and 15 minutes. You can gradually increase your time in bed on a weekly basis until you are no longer sleepy enough to sleep at least 85% of your time in bed. Once you are sleeping only 85%, that may be the longest time in bed that you should allow yourself. One warning: although this kind of sleep restriction is now a standard element of the cognitive-behavioral treatment of insomnia, it does produce more daytime sleepiness in the first few weeks of treatment, so caution is necessary when driving.
Most sleep experts also recommend that whatever bedtime you allow yourself, you should not go to bed if you do not feel sleepy. Moreover, if you awaken at night and no longer feel sleepy, get out of bed, and do not go back until you are sleepy again and expect to fall asleep. Even after being up during the night, you should get out of bed by your regular awakening time, because sleeping late tends to make the problem worse. Getting out of bed when you are not sleepy makes you sleepier the next night and helps maintain good sleep habits.
Almost all of us have stayed up entirely for a night or two, so we know that nothing terrible happens to us. Many of the patients I talk with say that they have slept only a few hours a night for years, and yet they are somehow terrified that losing sleep will harm them. Probably not. Remember that if anything, the short sleepers tend to live longer and often are less depressed. If you are willing to stay out of bed and amuse yourself somewhere else when you are not sleepy, soon you will stop worrying about sleep. If you lose a whole night’s sleep or part of a night, so what? It probably will be a minor problem at most, as long as you do not worry about it. When you do go to bed (because you are finally sleepy), you will have restored your confidence that you are likely to fall asleep, so the long-term problem resolves.
It is extremely common that depression, advanced sleep phase, or delayed sleep phase lead to poor sleep habits, and then the poor sleep habits become part of the problem. For this reason, it is important to observe good sleep habits when you are using bright light, in order to restore your sleep confidence. It has been shown specifically that sleep restriction can reduce depression.[87]
If bad sleep habits are part of your problem, commercial websites such as CBTforInsomnia.com![]()
![]() and SHUTi can give you more detailed pointers about how to correct sleep habits. (As this is written, the availability of SHUTi is in transition, so it would be best to look for it on the web when you need it.) DO NOT USE THE POPULAR SLEEPING PILLS: they are too dangerous. For more information about the risks of sleeping pills, you can look at my free website, The Dark Side of Sleeping Pills
and SHUTi can give you more detailed pointers about how to correct sleep habits. (As this is written, the availability of SHUTi is in transition, so it would be best to look for it on the web when you need it.) DO NOT USE THE POPULAR SLEEPING PILLS: they are too dangerous. For more information about the risks of sleeping pills, you can look at my free website, The Dark Side of Sleeping Pills![]()
![]() . Some of this information about good sleep habits is explained in more detail there.
. Some of this information about good sleep habits is explained in more detail there.
A New Theory: How Does Bright Light Work Biologically?
For many decades, dozens of research groups have tried to understand the biology predisposing to depression and mania. There are hundreds of theories. Study of artificial light effects on mood began in the 19th century, and relevant study of circadian abnormalities in depression began with Richter’s work commencing over 80 years ago. The evidence for circadian system involvement has gradually become more and more compelling. My colleagues and I have reviewed some of this background in a long review article that proposed circadian and photoperiodic mechanisms for depression, notably involving the hypothalamic suprachiasmatic nucleus influencing the pars tuberalis (a hypothalamic region at the hypothalamic-pituitary junction.)[88] A PowerPoint graphic presentation offers some animated illustrations.[89] Additional compelling data were published after our 2015 review in the past couple of years.[90]
To simplify, melatonin is a hormone that has regulated seasonal and light responses as early in biological evolution as the single-cell living organisms. Elaborate largely-similar mechanisms to adapt biological responses to the seasons developed in fish, birds, and mammals. In mammals, bright morning light falling on the eyes and stimulating the intrinsically photosensitive retinal ganglion cells leads through a complex system (transmitted through the suprachiasmatic nucleus) to suppressing morning melatonin secretion. If melatonin is not suppressed at dawn, melatonin inhibits a neurochemical chain reaction in pars tuberalis that would have promoted release of active thyroid hormone into the hypothalamus. Accordingly, light at dawn facilitates hypothalamic thyroid hormone actions that increase pituitary gonadotropin hormones and regulate the hypothalamic-pituitary-adrenal cortisol system. In this way, we imagine that hypothalamic thyroid activity, independent of thyroid gland regulation, promotes a normal or elevated mood and prevents depression. This may be the primary mechanism by which bright morning light protects and restores mood.
The timing of a person’s internal body clocks is also a factor. For example, evening people (which depressed people tend to be) spontaneously begin secreting melatonin later in the evening, and their melatonin is elevated later into the morning (see Chapter 6). If evening people arise too late and do not expose themselves to daylight early enough, their morning melatonin may suppress hypothalamic levels of active thyroid hormone and lead to depression. The longer nights of winter may also be a factor in winter depression, because dawn may come too late to properly suppress morning melatonin, since a depressed person arising at their normal time in winter might be up long before dawn. It follows that bright light administered soon after a depressed person has been arising (or a little before), by suppressing the morning melatonin, would reduce depression. Further, in accordance with the phase response curve described in Chapter 6, by advancing the times when melatonin secretion spontaneously commences and terminates, morning bright light may correct the delayed phases of those suffering depressions.
It is possible that excessive morning bright light may excessively advance the time when melatonin secretion is terminated in the early morning, leading to an excess of hypothalamic active thyroid hormone. Since it is well-known that excessive peripheral thyroid hormone can cause manic symptoms, it would not be surprising if morning bright light, when producing excessive phase advances, were a factor predisposing to mania caused by excessive hypothalamic thyroid hormone.
It may be more difficult to reconcile the pars tuberalis theory with depression related to advanced sleep phase symptoms. One possibility would be that early sleep leads to an early onset of transcription of the gene EYA3, which seems to be transcribed for only about 12 hours per day. EYA3 is part of the pathway triggering pars tuberalis induction of active thyroid hormone, but EYA3 transcription is suppressed nocturnally by melatonin. It appears that normally some EYA3 is transcribed in the morning after melatonin secretion terminates, leading to adequate hypothalamic active thyroid concentrations. However, if the circadian pattern of EYA3 transcription and its termination became more advanced than melatonin secretion is advanced, melatonin might excessively suppress morning EYA3 transcription, resulting in inadequate active thyroid hormone in the hypothalamus. This might explain how phase advances of a special sort lead to depression.
These theories of the biology of depression might begin to explain the well-documented associations between depression and delayed or advanced sleep phase syndromes and their responses to bright light.
About This ebook
I wrote this little book for the worldwide web, so that people in need could learn how to use light treatment. Much of the book is written in the same tone and language with which I have explained light treatment to my patients. I offer opinions and guidance even where the scientific proof is incomplete. People want a doctor’s best advice, even when we are not certain of everything.
This is not intended to be a scientific article, but it may be useful to physicians who want to learn more about light treatment and how to use it. For physicians and others who want more scientific facts, I have provided links to a large number of scientific references without attempting to document every opinion. This is my advice, so not every doctor will agree with everything. You can find many of the articles referenced at a medical library or by searching the web through the National Institutes of Health’s PubMed service or through a web browser search.[91]
You may make printed or electronic copies of this book for yourself or to give to family or friends without charge. I would be happy if this book can help lots of people. The materials are copyrighted ©1997–2019 by Daniel F. Kripke, M.D. and may not be used commercially for sale without permission.
About Dr. Kripke
Before retiring, Daniel F. Kripke, M.D. was a licensed physician. He has been certified by the American Board of Psychiatry and Neurology and is an emeritus professor of psychiatry at the University of California, San Diego. Dr. Kripke was elected a fellow of the American Psychiatric Association. In 1973, Dr. Kripke established one of the first sleep clinics in the United States at the San Diego VA Medical Center. Dr. Kripke has also been associated with the Scripps Clinic Viterbi Family Sleep Center, La Jolla, California. In 1981, Dr. Kripke published the first controlled clinical trial of bright light treatment. For almost 40 years, Dr. Kripke has been doing research on light treatment and treating patients with light. Dr. Kripke has co-authored hundreds of medical articles and has given invited lectures in 18 countries.
Dr. Kripke has now retired from practice and no longer consults with patients. Please do not contact Dr. Kripke for personal medical advice. A physician should not give personal advice to a patient the physician does not know, and the California Medical Board considers it unethical to provide mail or email medical advice to people who have not been examined. Treatment of depression is best obtained from a nearby psychiatrist. Patients with delayed sleep phase disorder or advanced sleep phase disorder might find help at a sleep center such as the Scripps Clinic Viterbi Family Sleep Center in La Jolla, California.[92]
If you have a sleep problem, you might also be interested in reading Dr. Kripke’s other ebook at www.DarkSideOfSleepingPills.com![]()
![]() Some of this material is repeated in both books.
Some of this material is repeated in both books.
Acknowledgment: I have been fortunate that my research has been supported for over 35 years, mainly by the U.S. National Institutes of Health (NIH) and the Department of Veterans Affairs. For two years, I did sleep research as a US Air Force medical officer, and later, agencies of the U.S. Army and Navy supported work of my laboratory. The Department of Psychiatry, the Sam and Rose Stein Institute for Research on Aging, and the Center for Chronobiology of the University of California, San Diego have also supported my research, as has the Weingart Foundation and the American Cancer Society. Recently, the Scripps Clinic Viterbi Family Sleep Center has been supporting some of my research, particularly the recent studies of risks associated with hypnotics, assisted by the help of generous gifts from private donors. Makers of wrist activity monitors, especially Ambulatory Monitoring, Inc. (the manufacturer of the Actillume and other actigraphs) and Minimitter-Respironics (makers of actigraphs, now part of Philips) have supported our research. Manufacturers of bright light treatment devices have supported our clinical research, especially The Sunbox Company, Apollo Health (now part of Philips), and Enviro-Med, partly through joint research projects funded by the National Institutes of Health. It is important that readers understand for whom an author has worked. Dr. Kripke and his family have no financial interest in any of the companies or products mentioned or in any commercial web site. Being supported largely by public funds, I have been able to speak out for public interests. I appreciate this opportunity, and have personally funded this nonprofit web site. - DFK
Notes for
Brighten Your Life
1. Espiritu, RC et al. Low illumination by San Diego adults: association with atypical depressive symptoms. Biol.Psychiatry. 1994;35:403-407; Kripke, DF et al. Adult illumination exposures and some correlations with symptoms, in Hiroshige T, Honma K (eds): Evolution of Circadian Clock. Sapporo, Hokkaido University Press; 1994:349-360. [return]
2. Cole, RJ et al. Seasonal variation in human illumination exposure at two different latitudes.
J.Biol.Rhythms. 1995![]()
![]() ;10:325-336. [return]
;10:325-336. [return]
3. Jean-Louis, G et al. Sleep duration, illumination, and activity patterns in a population sample: effects of gender and ethnicity. Biol.Psychiatry. 2000;47:921-927. [return]
4. Jean-Louis, G et al. Circadian sleep, illumination, and activity patterns in women: influences of aging and time reference. Physiology & Behavior. 2000; 68:347-352. [return]
5. Cole, RJ et al. Seasonal variation in human illumination exposure at two different latitudes.
J.Biol.Rhythms. 1995![]()
![]() ;10:325-336. [return]
;10:325-336. [return]
6. Youngstedt, SD et al. Light exposure, sleep quality, and depression in older adults. In Holick MF, Jung EG (eds): Biologic Effects of Light 1998. Boston, Kluwer Academic Publishers; 1999:427-435. [return]
7. Jean-Louis, G et al. Relationships among illumination, activity, and sleep patterns. In Holick MF, Jung EG (eds): Biological Effects of Light 1998. Boston, Kluwer Academic Publishers; 1999:37-39. [return]
8. Kessler, RC et al. Comorbidity of DSM-III-R major depressive disorder in the general population: Results
from the US National Comorbidity Survey. Br.J.Psychiatry. 1996;168:17-30; Murray CJ, Vos T, Lozano R, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012![]()
![]() ; 380(9859):2197-223. [return]
; 380(9859):2197-223. [return]
9. Pratt LA, Brody DJ, Gu Q. A. NCHS Data Brief No 283. Antidepressant Use Among Persons Aged 12 and Over: United States, 2011-2014. NCHS Data Brief No. 283 August 2017![]()
![]() . [return]
. [return]
10. Stone DM, Simon TR, Fowler KA, et al. Vital Signs: Trends in State Suicide Rates - United States, 1999-2016 and Circumstances Contributing to Suicide - 27 States, 2015. MMWR Morb Mortal Wkly Rep 2018![]()
![]() ;67(22):617-24.[return]
;67(22):617-24.[return]
11. Meehan, PJ et al. Suicides among older United States residents: epidemiologic characteristics and trends. Am.J.Public Health. 1991![]()
![]() ;81(9):1198-1200. [return]
;81(9):1198-1200. [return]
12. Kessler, RC et al. Prevalence, correlates, and course of minor depression and major depression in the national comorbidity survey. J.Affect.Dis. 1997;45:19-30. [return]
13. Kessler, RC et al. Comorbidity of DSM-III-R major depressive disorder in the general population: Results from the US National Comorbidity Survey. Br.J.Psychiatry. 1996;168:17-30. [return]
14. Kessler, RC et al. Comorbidity of DSM-III-R major depressive disorder in the general population: Results from the US National Comorbidity Survey. Br.J.Psychiatry. 1996;168:17-30. [return]
15. Lyness, JM et al. The importance of subsyndromal depression in older primary care patients: prevalence and associated functional disability. J.Am.Geriatr.Soc. 1999;47:647-652. [return]
16. Rosenthal, NE. Winter Blues (Seasonal Affective Disorder What It Is and How to Overcome It). New York, Guilford, 1993. [return]
17. Kitamura S, Hida A, Watanabe M, et al. Evening preference is related to the incidence of depressive states independent of sleep-wake conditions. Chronobiol Int 2010;27(9-10):1797-812; Vetter C, Chang SC, Devore EE, Rohrer F, Okereke OI, Schernhammer ES. Prospective study of chronotype and incident depression among middle- and older-aged women in the Nurses' Health Study II. J Psychiatr Res 2018;103:156-60. [return]
18. Schwartz, PJ et al. Winter seasonal affective disorder: A follow-up study of the first 59 patients of the National Institute of Mental Health Seasonal Studies Program. Am.J.Psychiatr. 1996;153:1028-1036. [return]
19. Kripke, DF et al. Adult illumination exposures and some correlations with symptoms. in Hiroshige T, Honma K (eds): Evolution of Circadian Clock. Sapporo, Hokkaido University Press; 1994:349-360. [return]
20. Kripke, DF. Light treatment for nonseasonal depression: speed, efficacy, and combined treatment. J.Affect.Dis. 1998;49:109-117; Beauchemin, KM et al. Phototherapy is a useful adjunct in the treatment of depressed in-patients. Acta Psychiatr Scand. 1997;95:424-427. [return]
21. Chang CH, Liu CY, Chen SJ, Tsai HC. Efficacy of light therapy on nonseasonal depression among elderly adults: a systematic review and meta-analysis Neuropsychiatr Dis Treat 2018![]()
![]() ; 2018(14):3091-102; Hopkins S, Morgan PL, Schlangen JM, Williams P, Skene J, Middleton B. Blue-enriched Lighting for Older People Living in Care Homes: Effect on Activity, Actigraphic Sleep, Mood and Alertness. Curr Alzheimer Res 2017;14(10):1053-1062.[return]
; 2018(14):3091-102; Hopkins S, Morgan PL, Schlangen JM, Williams P, Skene J, Middleton B. Blue-enriched Lighting for Older People Living in Care Homes: Effect on Activity, Actigraphic Sleep, Mood and Alertness. Curr Alzheimer Res 2017;14(10):1053-1062.[return]
22. Najjar RP, Zeitzer JM. Temporal integration of light flashes by the human circadian system. J Clin Invest 2016![]()
![]() ;126(3):938-47. [return]
;126(3):938-47. [return]
23. Terman, JS et al. Circadian time of morning light administration
and therapeutic response in winter depression. Arch Gen Psychiatry. 2001![]()
![]() ;58:69-75. [return]
;58:69-75. [return]
24. Wirz-Justice A, Terman M. Chronotherapeutics (light and wake therapy) as a class of interventions for affective disorders. Handb Clin Neurol 2012;106:697-713; Wirz-Justice A, Benedetti F, Terman M. Chronotherapeutics for Affective Disorders: A Clinician's Manual for Light and Wake Therapy. 2nd ed. Basel, Switzerland: Karger, 2013; Wu JC, Kelsoe JR, Schachat C, et al. Rapid and sustained antidepressant response with sleep deprivation and chronotherapy in bipolar disorder. Biol Psychiatry 2009;66(3):298-301. [return]
25. Benedetti F. Rate of switch from bipolar depression into mania after morning light therapy: A historical review. Psychiatry Res 2018;261:351-6; Sit DK, McGowan J, Wiltrout C, et al. Adjunctive Bright Light Therapy for Bipolar Depression: A Randomized Double-Blind Placebo-Controlled Trial. Am J Psychiatry. 2018![]()
![]() 175(2):131-9. [return]
175(2):131-9. [return]
26. The Society for Light Treatment and Biological Rhythms is a not-for-profit
international organization founded in 1988, dedicated to fostering research, professional
development and clinical applications in the fields of light therapy and biological
rhythms. A listing of SLTBR corporate members with light therapy products, and links to more information, may be found at the group’s website, www.sltbr.org![]()
![]() .[return]
.[return]
27. Duarte, D. Lamp’s labeling found to be fraudulent. FDA Talk 1986; 1-2. [return]
28. Avery, DH et al. Dawn simulation and bright light in the treatment of SAD: A controlled study. Biol Psychiatry. 2001;50:205-216. [return]
29. Lam RW, Levitt AJ, Levitan RD, et al. Efficacy of Bright Light Treatment, Fluoxetine, and the Combination in Patients With Nonseasonal Major Depressive Disorder: A Randomized Clinical Trial. JAMA Psychiatry 2016;![]()
![]() 73(1):56-63. [return]
73(1):56-63. [return]
30. Meyerhoff J, Young MA, Rohan KJ. Patterns of depressive symptom remission during the treatment of seasonal affective disorder with cognitive-behavioral therapy or light therapy. Depress Anxiety 2018;![]()
![]() 35(5):457-67. [return]
35(5):457-67. [return]
31. Rohan KJ, Meyerhoff J, Ho SY, Evans M, Postolache TT, Vacek PM. Outcomes One and Two Winters Following Cognitive-Behavioral Therapy or Light Therapy for Seasonal Affective Disorder. Am J Psychiatry 2016;![]()
![]() 173(3):244-51. [return]
173(3):244-51. [return]
32. Fournier, J. C., DeRubeis, R. J., Hollon, S. D., Dimidjian, S., Amsterdam, J. D., Shelton, R. C., and Fawcett, J. Antidepressant drug effects and depression severity: a patient-level meta-analysis. Journal of the American Medical Association. 303(1)![]()
![]() . 47-53, 2010. [return]
. 47-53, 2010. [return]
33. Mulrow, CD et al. Treatment of Depression: Newer Pharmacotherapies.
USPHS AHCPR, Rockville, MD, 1999. Evidence
Report/Technology Assessment No. 7![]()
![]() . AHCPR Publication No. 99-E014:1-2-32. [return]
. AHCPR Publication No. 99-E014:1-2-32. [return]
34. Canadian Consensus Guidelines for the Treatment of Seasonal Affective
Disorder. Clinical and Academic Publishing, Vancouver, 1999. The full
text is available for purchase at Amazon.com![]()
![]() . A summary of the report in PDF form is available at the website for Austrian light manufacturer Instantdaylight
. A summary of the report in PDF form is available at the website for Austrian light manufacturer Instantdaylight![]()
![]() . [return]
. [return]
35. Depression Guideline Panel. Depression in Primary Care: Volume 2. Treatment of Major Depression. Clinical Practice Guideline Number 5, U.S. Dept. HHS, AHCPR Publication 93-0551, 1993. [return]
36. Kripke, DF. Light treatment for nonseasonal depression: speed, efficacy, and combined treatment. J.Affect.Dis. 1998;49:109-117. [return]
37. Kripke, DF. Photoperiodic mechanisms for depression and its treatment. In, Perris C, Struwe G, Jansson B (eds): Biological Psychiatry. Elsevier-North Holland Biomedical Press; 1981, 1249-1252; Kripke, DF et al. Bright white light alleviates depression. Psychiatry Res.1983;10:105-112. [return]
38. Kripke, DF et al. Controlled trial of bright light for nonseasonal major depressive disorders. Biol.Psychiatry. 1992;31:119-134. [return]
39. Yamada, N et al. Clinical and chronobiological effects of light therapy on nonseasonal affective disorders. Biol Psychiatry. 1995;37:866-873. [return]
40. Mackert, A et al. Phototherapy in nonseasonal depression. Biol.Psychiatry. 1991; 30:257-268. [return]
41. Prasko, J et al. Hastened onset of the effect of antidepressive drugs when using three types of timing of intensive white light. Cs.Psychiat.1988; 84(6):373-383.; Schuchardt, HM et al. Lichttherapie in der psychiatrischen praxis. Fortschritte der Neurologie Psychiatrie. 1992;60(S2):193-194; Kasper, S et al. The effects of light therapy in treatment indications other than seasonal affective disorder (SAD). In, Holick MF, Jung EG (eds): Biologic Effects of Light 1993. Berlin, Walter de Gruyter; 1994:206-218. [return]
42. Reide, M et al. Light Therapy in the Treatment of Nonseasonal Major Depressive Disorder. In, Holick MF, Jung EG (eds): Biologic Effects of Light 1993. Berlin, Walter de Gruyter & Co.; 1994. [return]
43. Neumeister, A et al. Bright light therapy stabilizes the antidepressant effect of partial sleep deprivation. Biol Psychiatry. 1996;39:16-21. [return]
44. Bloching, B et al. Outlasting antidepressant effect of late partial sleep deprivation by bright light therapy. J.Sleep Res. 2000;9:21; Colombo, C et al. Total sleep deprivation combined with lithium and light therapy in the treatment of bipolar depression: replication of main effects and interaction. Psychiatry Res. 2000;95:43-53. [return]
45. Loving RT, Kripke DF, Shuchter SR. Bright light augments antidepressant
effects of medication and wake therapy. Depress
Anxiety. 2002![]()
![]() ;16(1):1-3. [return]
;16(1):1-3. [return]
46. Moffit, MT. Bright light treatment of late-life depression.
Thesis, UMI Dissertation Services #9326258. Sumaya, IC et al. Bright light
treatment decreases depression in institutionalized older adults: a placebo-controlled
crossover study. J
Gerontol A Biol Sci Med Sci. 2001![]()
![]() Jun;56(6):M356-60. Royer, M., Ballentine, H., Eslinger, P. J., Houser,
K., Mistrick, R., Behr, R., and Rakos, K. Light Therapy for Seniors in Long-Term
Care. J
Am Med Dir Assoc. 2012 Feb;13(2):100-2. Van der Lek RF, Swaab DF, Twisk J, Hol, EM, Hoogendijk,
W J, and van Someren, EJ. Effect of bright light and melatonin on cognitive and
noncognitive function in elderly residents of group care facilities: a randomized
controlled trial.
JAMA. 2008
Jun;56(6):M356-60. Royer, M., Ballentine, H., Eslinger, P. J., Houser,
K., Mistrick, R., Behr, R., and Rakos, K. Light Therapy for Seniors in Long-Term
Care. J
Am Med Dir Assoc. 2012 Feb;13(2):100-2. Van der Lek RF, Swaab DF, Twisk J, Hol, EM, Hoogendijk,
W J, and van Someren, EJ. Effect of bright light and melatonin on cognitive and
noncognitive function in elderly residents of group care facilities: a randomized
controlled trial.
JAMA. 2008![]()
![]() ;299(22):2642-2655. [return]
;299(22):2642-2655. [return]
47. Beauchemin, KM et al. Phototherapy is a useful adjunct in the treatment of depressed in-patients. Acta Psychiatr Scand. 1997;95:424-427. [return]
48. Beauchemin, KM et al. Sunny hospital rooms expedite recovery from severe and refractory depressions. J.Affect.Disord. 1996;40:49-51; Benedetti, F et al. Morning sunlight reduces length of hospitalization in bipolar depression. J.Affect.Disord. 2001;62:221-223. [return]
49. Lam, RW, Carter D, Misri S, Kuan AJ, Yatham LN, Zis AP. A controlled study of light therapy in women with late luteal phase dysphoric disorder. Psychiatry Res. 1999;86:185-192. [return]
50. Mackert, A et al. Phototherapy in nonseasonal depression. Biol.Psychiatry. 1991;30:257-268.; Fritzsche, M et al. Sleep deprivation as a predictor of response to light therapy in major depression. J.Affect.Disord. 2001;62:207-215. [return]
51. Holsboer-Trachsler, E et al. Sleep deprivation and bright light as potential augmenters of antidepressant drug treatment - neurobiological and psychometric assessment of course. J Psychiat Res. 1994;28:381-399. [return]
52. Lieverse R, van Someren E J, Nielen, MM, Uitdehaag, BM, Smit, JH,
and Hoogendijk, WJ. Bright light treatment in elderly patients with nonseasonal
major depressive disorder: a randomized placebo-controlled trial. Arch Gen.Psychiatry 68(1)![]()
![]() , 61-70. 2011. [return]
, 61-70. 2011. [return]
53. Martiny K, Lunde M, Unden M, Dam, H, and Bech, P. Adjunctive bright light in non-seasonal major depression: results from patient-reported symptom and well-being scales. Acta Psychiatr Scand. 2005 Jun;111(6):453-9; Martiny K, Lunde M, Unden M, Dam H, and Bech, P. Adjunctive bright light in non-seasonal major depression: results from clinician-rated depression scales. Acta Psychiatr Scand. 2005 Aug;112(2):117-25. [return]
54. Martiny, K., Refsgaard, E., Lund, V., Lunde, M., Sorensen, L., Thougaard, B., Lindberg, L., and Bech, P. A 9-week randomized trial comparing a chronotherapeutic intervention (wake and light therapy) to exercise in major depressive disorder patients treated with duloxetine. Journal of Clinical Psychiatry 73(9), 1234-1242. 2012. [return]
55. Canadian Consensus Guidelines for the Treatment of Seasonal Affective Disorder. Clinical and Academic Publishing, Vancouver, 1999. Lam, R.W. and Tam, E.M. A Clinician’s Guide to Using Light Therapy. New York, Cambridge University Press, 2009. [return]
56. Depression Guideline Panel. Depression in Primary Care: Volume 2. Treatment of Major Depression. Clinical Practice Guideline Number 5.1, U.S. Dept. HHS, AHCPR Publication 93-0551, 1993. [return]
57. Tuunainen A, Kripke DF, Endo T. Light therapy for non-seasonal depression.
Cochrane Database Syst
Rev. 2004![]()
![]() ;(2):CD004050. [return]
;(2):CD004050. [return]
58. Golden RN, et al. The efficacy of light therapy in the treatment
of mood disorders: a review and meta-analysis of the evidence. Am.J
Psychiatry 162(4)![]()
![]() , 656-662. 2005. [return]
, 656-662. 2005. [return]
59. Even C, Schröder CM, Friedman S, and Rouillon F. The efficacy of light therapy in nonseasonal depression: A systematic review. J Affect.Disord. 108, 11-23. 2008. [return]
60. Chang CH, Liu CY, Chen SJ, Tsai HC. Efficacy of light therapy on nonseasonal depression among elderly adults: a systematic review and meta-analysis [Corrigendum] Neuropsychiatr Dis Treat 2016![]()
![]() ; 26(6):1037-47; Perera S, Eisen R, Bhatt M, et al. Light therapy for non-seasonal depression: systematic review and meta-analysis. Eur Neuropsychopharmacol 2016
; 26(6):1037-47; Perera S, Eisen R, Bhatt M, et al. Light therapy for non-seasonal depression: systematic review and meta-analysis. Eur Neuropsychopharmacol 2016![]()
![]() ;2(2):116-26; Tseng PT, Chen YW, Tu KY, et al. Light therapy in the treatment of patients with bipolar depression: A meta-analytic study. Eur Neuropsychopharmacol 2016;26(6):1037-47; Zhao X, Ma J, Wu S, Chi I, Bai Z. Light therapy for older patients with non-seasonal depression: A systematic review and meta-analysis. J Affect Disord 2018;232:291-9.[return]
;2(2):116-26; Tseng PT, Chen YW, Tu KY, et al. Light therapy in the treatment of patients with bipolar depression: A meta-analytic study. Eur Neuropsychopharmacol 2016;26(6):1037-47; Zhao X, Ma J, Wu S, Chi I, Bai Z. Light therapy for older patients with non-seasonal depression: A systematic review and meta-analysis. J Affect Disord 2018;232:291-9.[return]
61. Lieverse R, van Someren EJ, Nielen MM, Uitdehaag, BM, Smit, JH, and Hoogendijk, WJ. Bright light treatment in elderly patients with nonseasonal
major depressive disorder: a randomized placebo-controlled trial. Arch Gen.Psychiatry 68(1)![]()
![]() , 61-70. 2011. [return]
, 61-70. 2011. [return]
62. Wirz-Justice A, Bader A, Frisch U, Stieglitz RD, Alder J, Bitzer J, Hosli I, Jazbec S, Benedetti F, Terman M, Wisner KL, and Riecher-Rossler A. A randomized, double-blind, placebo-controlled study of light therapy for antepartum depression. J Clin Psychiatry. 72:986-993, 2011. [return]
63. Wirz-Justice, A., Benedetti, F., and Terman, M. Chronotherapeutics for Affective Disorders: A clinician’s manual for light and wake therapy. 1-116. 2009. Basel, Karger. A second, revised edition of this manual was published in June 2013, ISBN 978-3-318-02090-8, and can be ordered through Karger Medical and Scientific Publishers, www.karger.com/Book/Home/257464.![]()
![]() ; Wu JC, Kelsoe JR, Schachat C, et al. Rapid and sustained antidepressant response with sleep deprivation and chronotherapy in bipolar disorder. Biol Psychiatry 2009;66(3):298-301.[return]
; Wu JC, Kelsoe JR, Schachat C, et al. Rapid and sustained antidepressant response with sleep deprivation and chronotherapy in bipolar disorder. Biol Psychiatry 2009;66(3):298-301.[return]
64. Rosenthal, NE et al. Seasonal affective disorder: a description of the syndrome and preliminary findings with light therapy. Arch.Gen.Psychiatry.1984;41:72-80. [return]
65. Meyerhoff J, Young MA, Rohan KJ. Patterns of depressive symptom remission during the treatment of seasonal affective disorder with cognitive-behavioral therapy or light therapy. Depress Anxiety![]()
![]() 2018;35(5):457-67; Lam RW, Levitt AJ, Levitan RD, et al. The Can-SAD study: a randomized controlled trial of the effectiveness of light therapy and fluoxetine in patients with winter seasonal affective disorder. Am J Psychiatry 2006;163(5):805-12[return]
2018;35(5):457-67; Lam RW, Levitt AJ, Levitan RD, et al. The Can-SAD study: a randomized controlled trial of the effectiveness of light therapy and fluoxetine in patients with winter seasonal affective disorder. Am J Psychiatry 2006;163(5):805-12[return]
66. Lam RW, Levitt AJ, Levitan RD, et al. Efficacy of Bright Light Treatment, Fluoxetine, and the Combination in Patients With Nonseasonal Major Depressive Disorder: A Randomized Clinical Trial. JAMA Psychiatry 2016;![]()
![]() 73(1):56-63; Lam RW, Levitt AJ, Levitan RD, et al. The Can-SAD study: a randomized controlled trial of the effectiveness of light therapy and fluoxetine in patients with winter seasonal affective disorder. Am J Psychiatry 2006;163(5):805-12[return]
73(1):56-63; Lam RW, Levitt AJ, Levitan RD, et al. The Can-SAD study: a randomized controlled trial of the effectiveness of light therapy and fluoxetine in patients with winter seasonal affective disorder. Am J Psychiatry 2006;163(5):805-12[return]
67. Schwartz, PJ et al. Winter seasonal affective disorder: A follow-up study of the first 59 patients of the National Institute of Mental Health Seasonal Studies Program. Am.J.Psychiatry. 1996; 153:1028-1036. [return]
68. Khan, A et al. Symptom reduction and suicide risk in patients treated with placebo in antidepressant clinical trials. Arch Gen Psychiatry. 2000;57:311-328. [return]
69. Storosum JG, Elferink AJ, van Zwieten BJ, van den Brink W, Gersons BP, van Strik R, Broekmans AW. Short-term efficacy of tricyclic antidepressants revisited: A meta-analytic study. Eur Neuropsychopharmacol. 2001 Apr;11(2):173-80. [return]
70. Bech, P et al. Meta-analysis of randomised controlled trials of fluoxetine v. placebo and tricyclic antidepressants in the short-term treatment of major depression. Brit.J.Psychiat.
2000![]()
![]() ;176:421-428. [return]
;176:421-428. [return]
71. Lam RW, Levitt AJ, Levitan RD, et al. Efficacy of Bright Light Treatment, Fluoxetine, and the Combination in Patients With Nonseasonal Major Depressive Disorder: A Randomized Clinical Trial. JAMA Psychiatry 2016;![]()
![]() 73(1):56-63. [return]
73(1):56-63. [return]
72. Mulrow, CD et al. Treatment of Depression: Newer Pharmacotherapies.
USPHS AHCPR, Rockville, MD, 1999. Evidence
Report/Technology Assessment No. 7![]()
![]() . AHCPR Publication No. 99-E014:1-2-32.[return]
. AHCPR Publication No. 99-E014:1-2-32.[return]
73. Fournier JC, DeRubeis RJ, Hollon SD, Dimidjian S, Amsterdam JD,
Shelton RC, and Fawcett J. Antidepressant drug effects and depression severity:
a patient-level meta-analysis. Journal
of the American Medical Association 303(1)![]()
![]() , 47-53, 2010. [return]
, 47-53, 2010. [return]
74. Kisely S, Li A, Warren N, Siskind D. A systematic review and meta-analysis of deep brain stimulation for depression. Depress Anxiety 2018![]()
![]() ;35(5):468-80. [return]
;35(5):468-80. [return]
75. Kripke DF, Elliott JA, Youngstedt SD, Rex KM. Circadian phase response curves to light in older and young women and men. J Circadian Rhythms. 2007![]()
![]() ; 5: 4. [return]
; 5: 4. [return]
76. Youngstedt, SD et al. Light exposure, sleep quality, and depression in older adults. in Holick MF, Jung EG (eds): Biologic Effects of Light 1998. Boston, Kluwer Academic Publishers; 1999:427-435. [return]
77. Avery, DH et al. Dawn simulation and bright light in the treatment of SAD: A controlled study. Biol Psychiatry. 2001;50:205-216. [return]
78. Cole, RJ et al. Bright light mask treatment of delayed sleep phase syndrome. Journal of Biological Rhythms. 2002![]()
![]() . [return]
. [return]
79. Jones SE, Lane JM, Wood AR, et al. Genome-wide association analyses of chronotype in 697,828 individuals provides insights into circadian rhythms. Nat Commun. 2019![]()
![]() ;10(1):343. [return]
;10(1):343. [return]
80. Benedetti F. Rate of switch from bipolar depression into mania after morning light therapy: A historical review. Psychiatry Res 2018;261:351-6; Sit DK, McGowan J, Wiltrout C, et al. Adjunctive Bright Light Therapy for Bipolar Depression: A Randomized Double-Blind Placebo-Controlled Trial. Am J Psychiatry. 2018![]()
![]() 175(2):131-9. [return]
175(2):131-9. [return]
81. Moon JH, Cho CH, Son GH, et al. Advanced Circadian Phase in Mania and Delayed Circadian Phase in Mixed Mania and Depression Returned to Normal after Treatment of Bipolar Disorder. EBioMedicine. 2016![]()
![]() ;11(Sep):285-95. [return]
;11(Sep):285-95. [return]
82. Leibenluft, E et al. Light therapy in patients with rapid cycling bipolar disorder: Preliminary results. Psychopharmacol.Bull. 1995![]()
![]() ;31:705-710; Sit DK, McGowan J, Wiltrout C, et al. Adjunctive Bright Light Therapy for Bipolar Depression: A Randomized Double-Blind Placebo-Controlled Trial. Am J Psychiatry. 2018
;31:705-710; Sit DK, McGowan J, Wiltrout C, et al. Adjunctive Bright Light Therapy for Bipolar Depression: A Randomized Double-Blind Placebo-Controlled Trial. Am J Psychiatry. 2018![]()
![]() 175(2):131-9. . [return]
175(2):131-9. . [return]
83. Kripke DF, Garfinkel L, Wingard DL, Klauber MR, Marler MR. Mortality associated with sleep duration and insomnia. Arch Gen Psychiatry. 2002![]()
![]() ;59:131-136 [return]
;59:131-136 [return]
84. Silva AA, Mello RG, Schaan CW, Fuchs FD, Redline S, Fuchs SC. Sleep duration and mortality in the elderly: a systematic review with meta-analysis. BMJ Open. 2019![]()
![]() ;in press [return]
;in press [return]
85. Low DV, Wu MN, Spira AP. Sleep Duration and Cognition in a Nationally Representative Sample of U.S. Older Adults. Am J Geriatr Psychiatry. In press 2019![]()
![]() . [return]
. [return]
86. Kripke DF, Langer RD, Elliott JA, Klauber MR, Rex KM. Mortality related to actigraphic long and short sleep. Sleep Med. 2011![]()
![]() ;12(1):28-33. [return]
;12(1):28-33. [return]
87. Epstein DR, Sidani S, Bootzin RR, Belyea MJ. Dismantling multicomponent behavioral treatment for insomnia in older adults: a randomized controlled trial. Sleep. 2012![]()
![]() ;35(6):797-805; Kalmbach DA, Cheng P, Arnedt JT, et al. Treating insomnia improves depression, maladaptive thinking, and hyperarousal in postmenopausal women: comparing cognitive-behavioral therapy for insomnia (CBTI), sleep restriction therapy, and sleep hygiene education. Sleep Med 2018;55:124-34.[return]
;35(6):797-805; Kalmbach DA, Cheng P, Arnedt JT, et al. Treating insomnia improves depression, maladaptive thinking, and hyperarousal in postmenopausal women: comparing cognitive-behavioral therapy for insomnia (CBTI), sleep restriction therapy, and sleep hygiene education. Sleep Med 2018;55:124-34.[return]
88. Kripke DF, Elliott JA, Welsh DK, Youngstedt SD. Photoperiodic and circadian bifurcation theories of depression and mania. F1000Res. 2015![]()
![]() ;4:107. [return]
;4:107. [return]
89. Kripke, DF. The beginning of light therapy. 12-21-2016. [return]
90. Jones SE, Lane JM, Wood AR, et al. Genome-wide association analyses of chronotype in 697,828 individuals provides insights into circadian rhythms. Nat Commun 2019![]()
![]() ;10(1):343; Kripke, D. F. When our body clocks run late: does it make us depressed? Ann Transl Med
;10(1):343; Kripke, D. F. When our body clocks run late: does it make us depressed? Ann Transl Med![]()
![]() 4(9), 178. 2016.[return]
4(9), 178. 2016.[return]
91. PubMed is a free internet resource that is developed and maintained by the National Center for Biotechnology Information (NCBI), at the U.S. National Library of Medicine (NLM), located at the National Institutes of Health (NIH). www.ncbi.nlm.nih.gov/pubmed/![]()
![]() Click on ‘Help’ on the PubMed home page to learn how to use the service. [return]
Click on ‘Help’ on the PubMed home page to learn how to use the service. [return]
92. More information about Scripps Clinic Viterbi Family Sleep Center in La Jolla, California, is available online at
www.scripps.org![]()
![]() , or by phoning (858) 554-8845. [return]
, or by phoning (858) 554-8845. [return]
Table of Contents
Brighten Your Life, in all its formats, including this eBook, copyright ©1997-2019 by Daniel F. Kripke, M.D. All rights reserved.